How I Do It: Transversalis Fascia Plane Block
Cite as: Tan J, Chin KJ. How I do it: transversalis fascia plane block . ASRA Pain Medicine News 2024;49. https://doi.org/10.52211/asra050124.008.
Introduction
The transversalis fascia plane (TFP) block is an ultrasound-guided abdominal wall block involving injection of local anesthetic into the plane between the transversus abdominis muscle (TAM) and the deeper investing transversalis fascia.1,2 The injection point is immediately superior to the iliac crest and close to where the posterior edge of internal oblique muscle (IOM) and TAM meet the quadratus lumborum muscle (QLM). The TFP block targets the ilioinguinal and iliohypogastric nerves at a proximal location along their course and provides analgesia in the territory of their branches (Figure 1). Clinical applications include treatment of acute pain after anterior iliac crest bone graft harvesting2, inguinal herniorraphy3-6, caesarean section7-10; and management of chronic post-herniorraphy pain.11
Anatomy
The ilioinguinal and iliohypogastric nerves are terminal branches of the anterior ramus of the L1 spinal nerve with occasional contribution from T12.12 They emerge from the lateral border of the psoas major muscle, inferior to the 12th rib, and travel over the ventral surface of QLM (Figure 1). Lateral to QLM, they initially run deep to TAM for a variable distance before ascending and piercing TAM to enter the transversus abdominis plane (TAP) between IOM and TAM.12 Both nerves continue to travel anteriorly in the TAP, immediately superior to the iliac crest, before ascending through IOM and external oblique muscle (EOM) to terminate in the subcutaneous tissues of the anterior abdominal wall in the inguinal and pubic regions. The nerves give off perforating branches along their course that innervate the surrounding musculoskeletal structures, including the superior border of the bony iliac crest. The exact location at which the nerves pierce TAM, IOM, and EOM and travel in the respective planes between the musculofascial layers of the abdominal wall varies greatly between individuals. This interindividual anatomic variability is the main reason for the inconsistent success rates in blocking these nerves with ultrasound-guided TAP blocks and landmark-guided ilioinguinal-iliohypogastric blocks.12
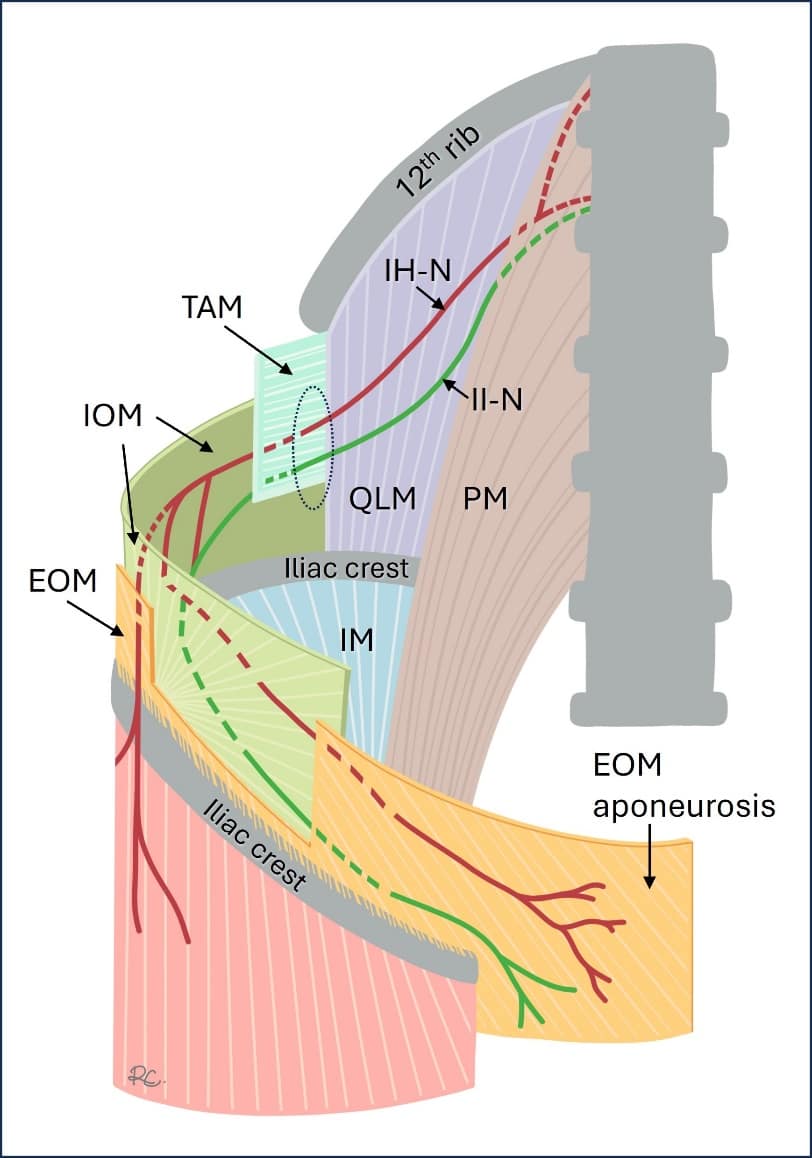
Figure 1. Anatomical course of the iliohypogastric nerve (IH-N) and ilioinguinal nerve (II-N) in relation to the muscular layers of the abdominal wall, which have been cut away for illustrative purposes. The IH-N and II-N emerge from the lateral edge of the psoas major muscle (PMM) and travel in an infero-lateral direction over the ventral surface of quadratus lumborum muscle. At this location (dotted circle), they are sandwiched between the deep fascia of TAM and the transversalis fascia (not shown); this is the target for injection in the transversalis fascia plane block. Both nerves gradually ascend through the muscular layers of the anterolateral abdominal wall, piercing each layer at a location that varies greatly between individuals. The IH-N and II-N supply branches (not shown) to the bony iliac crest as they course along its superior margin. They also innervate the other musculoskeletal structures through which they travel with terminal cutaneous branches in the inguinal and suprapubic region of the abdomen as well as over the supratrochanteric region of the hip.
EOM = external oblique muscle, IM = iliacus muscle, IOM = internal oblique muscle.
Used with permission: KJ Chin Medicine Professional Corporation
The TFP block targets the ilioinguinal and iliohypogastric nerves where they are consistently located deep to the posterior edge of TAM and before they ascend into the TAP. It also blocks the nerves proximal to the origin of their lateral cutaneous branches and branches to the iliac crest, increasing the area of coverage compared to a traditional ilioinguinal-iliohypogastric block. At this location, both nerves lie between the investing fascia of TAM and the transversalis fascia.12 The transversalis fascia is a thin aponeurotic membrane that is part of the larger endoabdominal fascia that lines the entire internal aspect of the abdominal wall and separates it from the parietal peritoneum.12 The transversalis fascia is continuous with fascia iliaca inferiorly and with the investing fascia of QLM and psoas major muscle medially (Figure 2).12 The fat-filled retroperitoneal cavity, and not the peritoneal cavity, lies deep to the tapered posterior edge of the TAM. The TFP block is performed immediately adjacent to the iliac crest in a transverse plane, which is inferior to the lower pole of the kidney. Together these factors minimize the risk of visceral injury.

Figure 2. Transverse section of the abdomen demonstrating the relationship of the transversalis fascia to the various musculofascial layers of the abdominal wall.
Block Technique
Positioning and Preparation
The TFP block may be performed with the patient in a supine or lateral decubitus position; however, we recommend the latter for better block ergonomics. A curvilinear transducer is generally recommended in adults as the wider field of view facilitates recognition of sonoanatomy, and the lower beam frequency provides better-quality images at tissue depths exceeding 4-5 cm. Obtaining crisp echogenic delineation of muscle borders and fascial planes is more important than resolution per se. However, in slim adults or pediatric patients, a high-frequency linear transducer will often provide good images and can be used instead. In adult patients, we recommend using an 80-100 mm needle and 20 ml of local anesthetic to achieve spread that will consistently reach the ilioinguinal and iliohypogastric nerves.
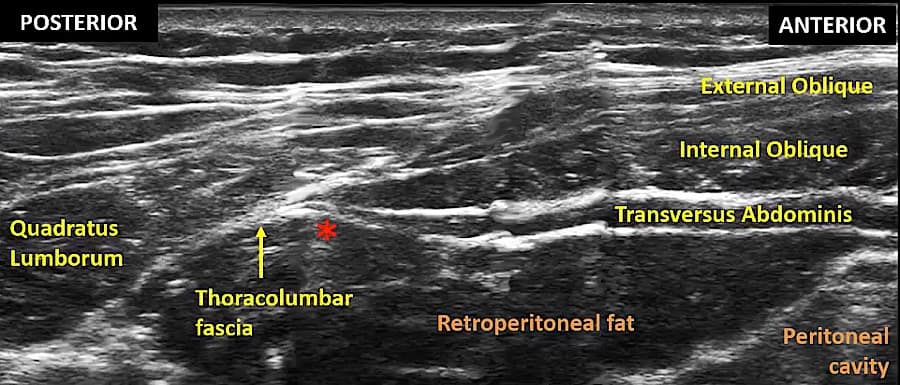
Identification of Sonoanatomy
Place the probe in a transverse orientation just superior to the iliac crest in the mid-axillary line to visualize the three muscular layers of the lateral abdominal wall. From superficial to deep, these are the EOM, IOM (usually the thickest layer), and TAM (usually the thinnest and darkest in appearance). Slide the probe posteriorly to visualize the posterior edge of IOM and TAM where they taper off into their common aponeurosis and border on the QLM (Figure 3).13 The dark hypoechoic area deep to the tapered posterior edge of the TAM is the fat-filled retroperitoneal space and not the intraperitoneal cavity. Tilting the probe slightly caudad into the pelvis often improves the clarity of the fascial borders of the tapered edge of TAM. The target for needle tip placement is just below the deep fascial layer of TAM close to its posterior edge (asterisk in Figure 3).13
Needle Insertion
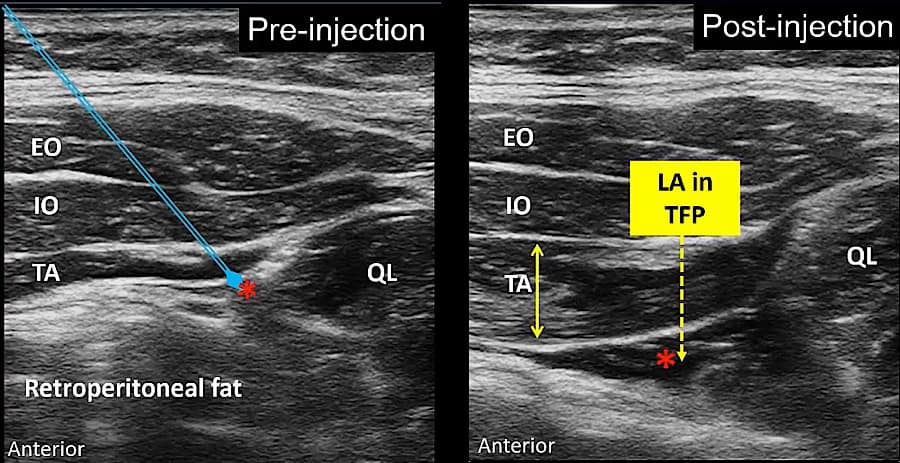
The needle is inserted in an anterior-to-posterior direction in a trajectory that passes through the tapered edge of TAM. Inserting the needle through muscle, rather than aiming for the hyperechoic confluence of fascial planes at the very edge of TAM, facilitates both tactile and visual recognition of needle tip entry into the correct fascial plane. Piercing the fascia between IOM and TAM produces a tactile pop plus visual stretch and rebound of the tissue layer. The needle is advanced through TAM to pierce the deep fascia of TAM, which will be signaled by similar tactile and visual feedback. A 0.5 ml test injection is then performed to confirm needle tip position.
The TFP block targets the ilioinguinal and iliohypogastric nerves where they are consistently located deep to the posterior edge of TAM and before they ascend into the TAP.
Correct placement between the deep fascia of TAM and the transversalis fascia will result in a visible pocket of fluid that peels the retroperitoneal fat away from the fascia, pushing the fat layer downwards (Figure 4).
If the needle tip has advanced too deep beyond the transversalis fascia, a swirling pattern of fluid spread within the retroperitoneal fat will be seen instead without the creation of a discrete fluid pocket. The needle should be withdrawn slightly, and the test injection repeated.
Conversely, if the needle tip has not advanced deep enough to fully pierce the deep fascia of TAM, the test injection will be intramuscular and distend TAM. The needle should be carefully advanced one fascial pop deeper, and the test injection repeated. These injection endpoints are illustrated in the figures below and in the video on the TFP block created by Professor Chin.13 Once the correct spread pattern has been obtained, the total injectate volume is delivered in this location.
Differences Between the TFP Block and Lateral Quadratus Lumborum (QL) Block and Posterior TAP Block
At a glance, the TFP block may appear very similar to a lateral quadratus lumborum (QL) block. The latter is also performed where TAM tapers off into thoracolumbar fascia and abuts against QLM.14 However, there are important and subtle differences between the two techniques. First, the TFP block is specifically designed to target the ilioinguinal and iliohypogastric nerves (L1 branches) and cover the iliac crest and inguinal region, whereas the lateral QL block is more often employed to primarily cover the flank and infraumbilical region of the abdominal wall in the territory of T10-T12 spinal nerves. If performing a lateral QLB, the probe is, therefore, often placed more superiorly, closer to the costal margin, compared to the TFP block. Second, the primary endpoint in the lateral QL block is LA spread around QLM rather than deep to TAM. Compared to the TFP block, the advocated needle tip placement in the lateral QL block is thus usually slightly more posterior at the confluence of thoracolumbar fascia and the QLM, and the needle trajectory generally does not pass through TAM.
The TFP block is also distinct from the posterior TAP block both in technical details and the expected clinical effect. The needle insertion endpoint for the posterior TAP is towards the tapered edge of IOM and TAM, but in the TAP, superficial rather than deep to TAM. Like the lateral QL block, the posterior TAP block is generally performed to target the anterolateral branches of the T10-T12 thoracoabdominal nerves and cover the infraumbilical abdominal wall. It may not reliably block the ilioinguinal and iliohypogastric nerves due to interindividual variability in their course within the TAP.15
Clinical Indications
The TFP block improves analgesia and reduces opioid consumption for post-surgical pain involving the iliac crest and T12-L1 spinal nerve territories. This includes iliac crest bone graft harvesting,2 inguinal herniorraphy,3-6 open appendectomy,16 chronic post-herniorraphy pain11 and caesarean section.7-10
Anterior Iliac Crest Bone Graft Harvest
TFP has been shown to reduce postoperative opioid consumption and pain scores after anterior iliac crest bone graft harvest in the immediate postoperative period.2 This block is also amenable to catheter insertion and has been used for anterior iliac crest bone graft harvest analgesia in pediatrics.17
Inguinal Hernia Repair
The TFP block improves pain scores and reduces opioid requirements for inguinal hernia repair in both adults and children.3-6 Compared to the transmuscular QL block, the TFP is as effective in reducing pain scores and opioid consumption; however, it may be technically easier and quicker to perform.4-5 Compared to the anterior TAP block, the TFP achieved a higher level of sensory block and reduced pain scores for inguinal hernia repair; however, there were no differences in opioid requirements.6
Cesarean Section
The TFP block improves early analgesia and opioid consumption and reduces postoperative nausea and vomiting in lower segment cesarean section (LSCS) where intrathecal morphine has not been used and is superior to wound infiltration.7-9 There is some early data suggesting it may reduce the incidence of chronic postsurgical pain compared to wound infiltration.9,10
Hip Surgery with Incisions in the L1 Territory
The TFP block is as effective as the QLB3 over control for reducing pain scores at rest and on movement in open hip repair of developmental dysplasia in pediatric patients and was superior to the QLB3 in this study for prolonging time to first analgesic request and reducing overall opioid consumption.18 The TFP block anesthetizes skin proximal to the lateral femoral cutaneous nerve (LFCN) block and thus improves coverage of proximal surgical incisions for hip surgery compared to LFCN block alone.19
Safety Considerations
Potential complications are like that of other ultrasound-guided abdominal wall blocks and include vascular injury, local anesthetic systemic toxicity, and risk of visceral injury. However, the risks of these are low if proper technique is observed, especially since viscera do not lie in the needle trajectory.2 There has been one report of quadriceps weakness after TFP, which is believed to have been caused by proximal spread of local anesthetic to the lumbar plexus; however, this is rarely observed in practice.20 Like most fascial plane blocks, the TFP is safe in coagulopathic patients, and there is little risk of needle-nerve injury as discrete nerves are not targeted.
Conclusion
The TFP block targets proximal blockade of the ilioinguinal and iliohypogastric nerves from the T12 and L1 spinal nerves by injecting local anesthetic between posterior aponeurotic extension of the TAM and deeper investing transversalis fascia. It is beneficial for analgesia in anterior iliac crest bone graft harvest, inguinal hernia repair, cesarean section, and hip surgery with incisions in the L1 territory. As a fascial plane block, it is safe in coagulopathy, and there is little risk of needle-nerve injury.

References
- Hebbard PD. Transversalis fascia plane block, a novel ultrasound-guided abdominal wall nerve block. Can J Anaesth 2009;56:618-20; https://doi.org/10.1007/s12630-009-9110-1
- Black ND, Malhas L, Jinet R, et al. The analgesic efficacy of the transversalis fascia plane block in iliac crest bone graft harvesting: a randomised controlled trial. Korean J Anesthesiol 2019;72(4):336-43. https://doi.org/10.4097/kja.d.18.00352
- Abdelbaser I, Mageed NA, El-Emam EM, et al. Preemptive analgesic efficacy of ultrasound-guided transversalis fascia plane block in children undergoing inguinal herniorrhaphy: a randomised, double-blind, controlled study. Korean J Anesthesiol 2021;74(4):325-32. https://doi.org/10.4097/kja.20601
- Abdelbaser I, Salah DM, Ateyya AA, et al. Ultrasound-guided transversalis fascia plane block versus lateral quadratus lumborum plane block for analagesia after inguinal herniotomy in children: a randomised controlled non-inferiority study. BMC Anesthesiol 2023;23(1):82. https://doi.org/10.1186/s12871-023-02043-x
- Fouad AZ, Abdel-Aal IRM, Ali Gadelrab MRM, et al. Ultrasound-guided transversalis fascia plane block versus transmuscular quadratus lumborum block for post-operative analgesia in inguinal hernia repair. Korean J Pain 2021;34(2):201-9. https://doi.org/10.3344/kjp.2021.34.2.201
- Lopex-Gonzalez JM, López-Álvarez S, Jiménez Gómez BM, et al Ultrasound-guided transversalis fascia plane block versus anterior transversus abdominis plane block in outpatient inguinal hernia repair. Rev Esp Anestesiol Reanim 2016;63(9):498-504. https://doi.org/10.1016/j.redar.2016.02.005
- Aydin, M.E. et al Subarachnoid block and ultrasound-guided transversalis fascia plane block for caesarean section: a randomised, double-blind, placebo-controlled trial. European Journal of Anaesthesiology. 2020;37(9)765-72. https://doi.org/
- Serifsoy, T.E. et al Evaluation of ultrasound-guided transversalis fascia plane block for postoperative analgesia in cesarean section: A prospective, randomized, controlled clinical trial. Journal of clinical anesthesia. 2020;59:56-60. https://doi.org/
- Chilkoti GT, Gaur D, Saxenaet AK, al Ultrasound-guided transversalis fascia plane block versus wound infiltration for both acute and chronic post-caesarean pain management – a randomised controlled trial. Indian J Anaesth 2022;66(7):517-22. https://doi.org/10.4103/ija.ija_173_22
- Borys M, Potręć-Studzińska B, Wiech M, et al. Transversus abdominis plane block and quadratus lumborum block did not reduce the incidence or severity of chronic postsurgical pain following cesarean section: a prospective, observational study.
- Choudhary J, Mishra AK, Jadhav R. Transversalis fascia plane block for the treatment of chronic postherniorrhaphy inguinal pain: a case report. A A Pract 2018;11(3):57-9. https://doi.org/10.1213/XAA.0000000000000730
- Chin et al Essentials of our current understanding: abdominal wall blocks. Reg Anesth Pain Med 2017;42:133-83. https://doi.org/10.1097/AAP.0000000000000545
- Chin, KJ. US-Guided Transversalis Fascia Plane (TFP) Block. 2020. https://youtu.be/bzx9Vpkgl8U.
- Elsharkawy H, El-Boghdadly K, Barrington M. Quadratus lumborum block: anatomical concepts, mechanisms, techniques. Anesthesiology 2019;130(2):322-35.https://doi.org/10.1097/ALN.0000000000002524
- Lee TH, Barrington MJ, Tran TMN, et al. Comparison of extent of sensory block following posterior and subcostal approaches to ultrasound-guided transversus abdominis plane block. Anaesth Intensive Care 2010;38:452-60. https://doi.org/10.1177/0310057X1003800307
- Nair A, Dudhedia U, Rangaiah M, et al. Ultrasound-guided transversalis fascia plane block for postoperative analgesia: asystematic review and meta-analysis. Indian J Anaesth 2023;67(4):331-42. https://doi.org/10.4103/ija.ija_43_23
- Sequera-Ramos L, Ruby JM, Jackson OA, et al. Continuous transversalis fascia plane catheter infusion in a pediatric patient undergoing alveolar cleft repair with iliac crest bone graft: a case report. A A Pract 2019;13(5):162-5. https://doi.org/10.1213/XAA.0000000000001013
- Huang C, Zhang X, Dong C, et al. Postoperative analgesic effects of the quadratus lumborum block 3 and transversalis fascia plane block in paediatric patients with developmental dysplasia of the hip undergoing open reduction surgeries: a double-blinded randomised controlled trial. BMJ Open2021;11(2):e038992. https://doi.org/10.1136/bmjopen-2020-038992
- Neilsen TD, Moriggl B, Barckman J, et al. Cutaneous anaesthesia of hip surgery incisions with iliohypogastric and subcostal nerve blockade: a randomized trial. Acta Anaesthesiol Scand2019;63(1):101-10. https://doi.org/10.1111/aas.13221
- Lee S, Goetz T, Gharapetian A. Unanticipated motor weakness with ultrasound-guided transversalis fascia plane block. A A Case Rep 2015;5(7):124-5. https://doi.org/1213/XAA.0000000000000237