Suprascapular Nerve Block
Authors
Philip Peng, MBBS, FRCPC
Associate Professor
Rachael Seib, MD
Resident Physician
Department of Anesthesia
University of Toronto
Toronto, Ontario, Canada
Commentary
Bernhard Moriggl, MD
Professor
Innsbruck Medical University
Innsbruck, Austria
Introduction
Suprascapular nerve (SSN) block, first described in 1941,[1] is indicated for management of acute perioperative pain and a variety of chronic pain in the shoulder. The indications include adhesive capsulitis, frozen shoulder, rotator cuff tear, and degenerative or inflammatory glenohumeral arthritis.[2-6] It is also performed as a diagnostic block for suprascapular neuropathy.[7]
Anatomy
The SSN originates from the superior trunk (C5 and C6) of the brachial plexus, runs parallel to the omohyoid muscle, and courses posteriorly under the trapezius muscle before it passes under the transverse scapular ligament in the suprascapular notch (Figure 1). It then passes beneath the supraspinatus muscle, and curves around the lateral border of the spine of the scapula (spinoglenoid notch) to the infraspinatous fossa (Figure 2).[2] In the supraspinatous fossa it gives off two branches, one to the supraspinatus muscle and one to the shoulder joint as an articular branch. In the infraspinatous fossa it gives off branches to the infraspinatous muscle, and to the shoulder joint and scapula. The sensory component of the SSN provides innervation to approximately 70% of the shoulder joint. The SSN does not have a significant cutaneous branch.
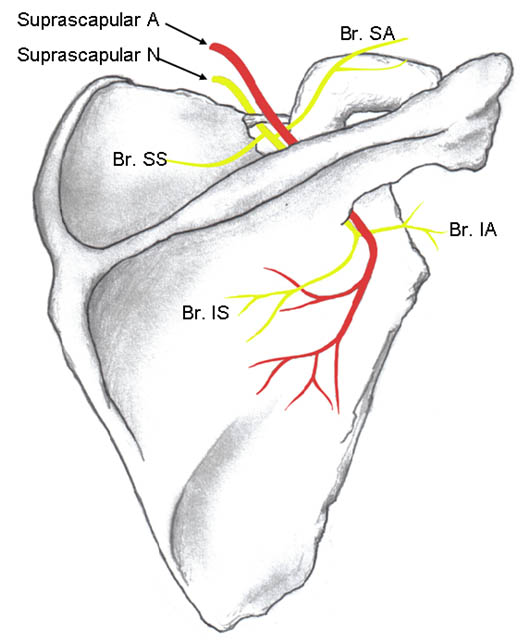 Figure 1. Suprascapular nerve and its branches. The superior articular branch (Br. SA) supplies the coracohumeral ligament, subacromial bursa and posterior aspect of the acromioclavicular joint capsule. The inferior articular branch (Br. IA) supplies the posterior joint capsule. Br. SS = branch to the supraspinatus muscle; Br. IS = branch to the infraspinatus muscle. Reproduced with permission form USRA (www.usra.ca)
Figure 1. Suprascapular nerve and its branches. The superior articular branch (Br. SA) supplies the coracohumeral ligament, subacromial bursa and posterior aspect of the acromioclavicular joint capsule. The inferior articular branch (Br. IA) supplies the posterior joint capsule. Br. SS = branch to the supraspinatus muscle; Br. IS = branch to the infraspinatus muscle. Reproduced with permission form USRA (www.usra.ca)
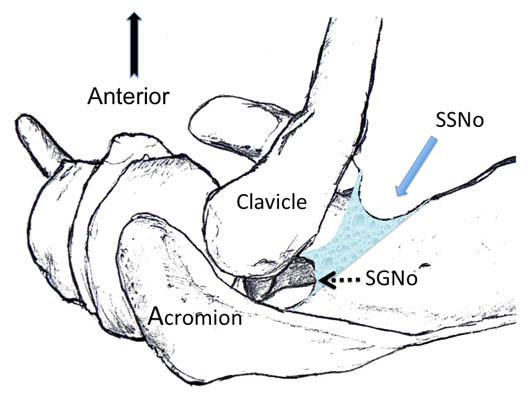
Figure 2. Superior view of the left shoulder. The suprascapular nerve enters the suprascapular fossa through the suprascapular notch (SSNo) and then courses into the infrascapular fossa through the spinoglenoid notch (SGNo). Reproduced with permission from USRA (www.usra.ca)
The ‘U’ or ‘V’ shaped suprascapular notch is located on the superior margin of the scapula, medial to the coracoid process (Figure 1). However, the notch is absent in up to 8% of cadavers.[8] Above the transverse scapular ligament run the suprascapular artery and vein, although rarely the artery travels along with the suprascapular nerve through the notch. The supraspinous fossa is bordered by the spine of the scapula dorsally, by the plate of the scapula ventrally and by the supraspinatus fascia superiorly, forming a classic compartment, the only exit through which is the suprascapular fossa.
Traditional Technique
The targets for most of the techniques are either at the suprascapular notch or on the floor of the scapular spine.[2] With the notch as the target, there are potentials for SSN block failure and/or adverse effects especially if image guidance is not used. The risk of pneumothorax is approximately 1% and this complication usually arises from the needle being inserted too deep.[9-10] If the needle is placed blindly into the notch, the needle tip is unlikely to approximate the notch as demonstrated by a study using CT to confirm the position of the needle.[11-12] With the use of fluoroscopy, the position of the needle in the notch can be assured. However, there is a potential of spilling of local anesthetic to the brachial plexus.[13]
A superior approach has been described in which the needle is inserted vertically into the suprascapular fossa. Large volumes of solution (10 mL or more) will accomplish this, but according to a recent study in cadavers, there will be spread to the axillary fossa in a minority of these cases.[13]
Ultrasound Technique
Sonoanatomy
The ideal site to perform the SSN injection is at the floor of the scapular spine between the suprascapular notch and spinoglenoid notch (Figure 2).[14] First, this technique is independent of the notch as a target. Thus, it avoids the risk of pneumothorax if one considers the direction of the needle. This technique is also feasible in individuals without a suprascapular notch (8% of the population). Second, the suprascapular fossa forms a compartment to retain the injected local anesthetic around the nerve even with a small volume.[13] In contrast, depositing local anesthetic at the notch level will result in the spread of local anesthetic to the brachial plexus.[13] Third, while imaging the suprascapular notch is possible, advancing the needle perfectly in plane in this orientation is very challenging (Figure 3 A, B). A slight deviation in the anterior direction will direct the needle towards the thorax.
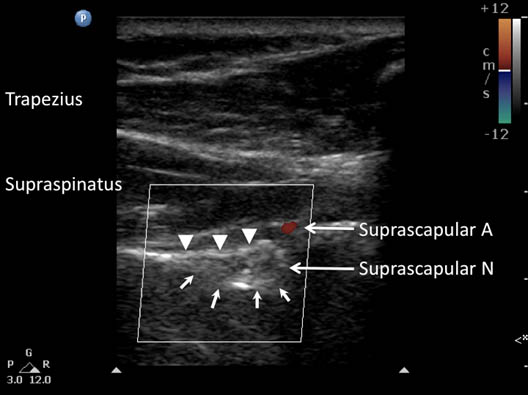
Figure 3A. Ultrasonographic image of the suprascapular nerve in the suprascapular notch (arrows). Note that at this level, the suprascapular artery is above the transverse scapular ligament (arrowheads). A = artery; N = nerve. Reproduced with permission form USRA (www.usra.ca).

Figure 3B. Ultrasonographic image of the suprascapular nerve slightly posterior to the plane obtained in 3A. The suprascapular artery is seen running towards the floor of the scapular spine. Note that a slight anterior needle deviation can potentially slide the needle towards the thorax. Reproduced with permission from USRA (www.usra.ca).
Scanning Technique
When imaging the suprascapular fossa with the ultrasound, the two key muscles in the scan are the trapezius and supraspinatus muscles (Figure 4). The suprascapular nerve is often seen accompanied by the suprascapular artery on the floor of the scapular spine between the suprascapular notch and spinoglenoid notch. The scapula spine forms an angle (39.50 ± 5.80) to the axis of the scapula blade[15] thus orientation of the ultrasound transducer should be closer to the coronal plane in order to visualize the contents of the suprascapular fossa.
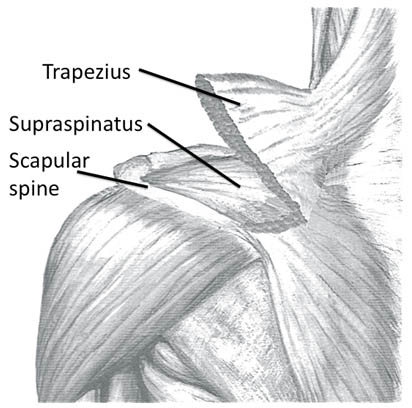 Figure 4. Left shoulder showing the muscle layers in the suprascapular fossa. Reproduced with permission from USRA (www.usra.ca)
Figure 4. Left shoulder showing the muscle layers in the suprascapular fossa. Reproduced with permission from USRA (www.usra.ca)
Block Technique
The patient can be sitting or prone. The scapula spine, coracoid process and acromion are used as palpable landmarks. Ultrasound scanning is performed with a linear ultrasound transducer (7-13 MHz) placed in a coronal plane over the suprascapular fossa with a slight anterior tilt. The transducer is oriented such that it is perpendicular to the line joining the coracoid process and the acromion (reflecting the position of the spinoglenoiod notch). The supraspinatus and trapezius muscles and the bony fossa underneath them should come into view (Figure 5). By adjusting the angle of the ultrasound transducer in a cephalo-caudad direction, the suprascapular nerve and artery should be brought into view in the trough of the floor. The nerve can sometimes be difficult to visualize as it has an approximate diameter of 25 mm.[19]
A 22-gauge, 80-mm needle is inserted either in-plane or out of plane, although the authors prefer to place the needle with an in-plane technique from the medial aspect of the transducer as the presence of the acromion process on the lateral side makes it difficult to angulate the needle. Because of the proximity of the nerve, an injectate volume of 5-8 mL is usually sufficient.
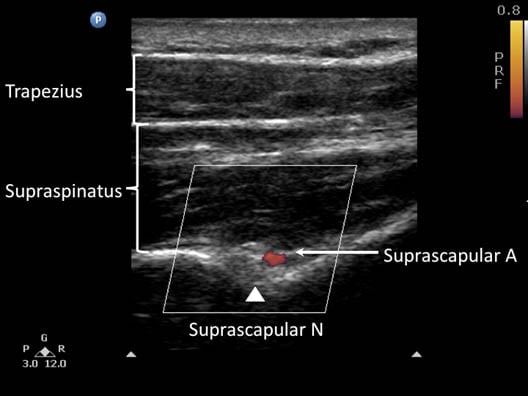 Figure 5. Ultrasonographic image of the suprascapular nerve on the floor of the scapular spine between suprascapular notch and spinoglenoid notch. Both suprascapular nerve and artery run underneath the fascia of supraspinatus muscle. Reproduced with permission from USRA (www.usra.ca)
Figure 5. Ultrasonographic image of the suprascapular nerve on the floor of the scapular spine between suprascapular notch and spinoglenoid notch. Both suprascapular nerve and artery run underneath the fascia of supraspinatus muscle. Reproduced with permission from USRA (www.usra.ca)
Literature Review
The sonoanatomy of the SSN relevant to nerve block injection and the injection techniques have been described recently.[16-18] Of interest, two of these articles[16-17] described the technique directing the needle to the scapular notch. However, description of the ultrasound transducer position and the sonograms strongly suggested that the SSN images were captured on the floor of the scapular spine. The third article demonstrated SSN sonoanatomy with the transducer positioned in the coronal plane with a slight anterior tilt.
Commentary
Classification of Procedure
This is considered an intermediate (level 2) block because the target structure lies relatively deep. Also, direct visualization of the nerve may be impaired because of bony artifacts since the nerve lies directly on bone.
Transducer Frequency
A lower frequency curved arrayed transducer may be necessary in patients who are very muscular or obese. In this case, nerve visibility is not guaranteed when scanned with a lower frequency transducer.
Additional Remarks
The SSN is a thick nerve, arising from the upper margin of the superior trunk of the brachial plexus. Between the scapular foramen (notch) and the spinoglenoid notch, the nerve is in direct contact with bone. The course within the supraspinatus fossa is considerably oblique and this has an important impact on scanning and correct transducer positioning. For example, the transducer needs to be positioned oblique in order for the ultrasound beam to be perpendicular to the course of the nerve.
Both the scapular notch (if present) and the spinoglenoid notch can easily be identified sonographically. It is important to point out that the notches are not the site of SSN blockade. The optimal site of SSN blockade is at the bottom of the supraspinatus fossa half way between the scapular notch and the spinoglenoid notch, i.e., at the superior part of the neck of the scapula. The SSN is mostly oval in shape but is variable in sonographic appearances, ranging from hyperechoic to hypoechoic.
The common mistakes for performing a SSN block are: 1) inappropriate transducer positioning (e.g. parallel to spine of scapula or in line with the supraspinatus muscle); 2) use of a transducer with appropriately high frequency when the subject is obese; 3) error in identifying the superior transverse suprascapular ligament; and 4) error in identifying the scapular notch and the spinoglenoid notch.
An alternative approach is to block the SSN at the origin where it branches off the superior trunk of the brachial plexus in the posterior triangle of neck. There are no external landmarks for this alternative approach. A sitting or supine patient position and a linear high frequency transducer (as high as possible) are recommended. One key easily identified internal landmark is the omohyoid muscle as the nerve passes underneath this muscle and then they run together towards the suprascapular notch. The SSN is typically hypoechoic and round or oval in shape.
References
- Wertheim HM, Rovenstine EA. Suprascapular nerve block. Anesthesiology 1941;2:541-545.
- Peng P, Narouze S. Ultrasound-guided interventional procedures in pain Medicine: A review of anatomy, sonoanaotmy and procedures. Part I: Non-axial structures. Reg Anesth Pain Med 2009;34:458-474.
- Ritchie ED, Tong D, Chung F, et al. Suprascapular nerve block for postoperative pain relief in arthroscopic shoulder surgery: A new modality? Anesth Analg 1997;84:1306-1312.
- Wassef MR. Suprascapular nerve block. A new approach for the management of frozen shoulder. Anaesthesia 1992;47:120-4.
- Karatas GK, Meray J. Suprascapular nerve block for pain relief in adhesive capsulitis: comparison of 2 different techniques. Arch Phys Med Rehabil 2002;83:593-7.
- Brown DE, James DC, Roy S: Pain relief by suprascapular nerve block in gleno-humeral arthritis. Scand J Rhematology 1988;17:411-415.
- Tubbs RS, Smyth MD, Salter G, et al: Anomalous transversement of the suprascapular artery through the suprascapular notch: a possible mechanism for undiagnosed shoulder pain? Med Sci Monit 2003;9:116-119.
- Natsis K, Totlis T, Tsikaras P, Appell HJ, Skandalakis P, Koebke J. Proposal for classification of the suprascapular notch: a study on 423 dried scapulas. Clin Anat 2007;20:135-139.
- Moore DC: Block of the suprascapular nerve. In: Thomas CC, ed: Regional nerve block. Springfield, MA, 1979;300-303.
- Dangoisse MJ, Wilson DJ, Glynn CJ: MRI and clinical study of an easy and safe technique of suprascapular nerve blockade. Acta Anaesth Belg 1994;45:49-54.
- Schneider-Kolsky ME, Pike J, Connell DA: CT-guided suprascapular nerve blocks: a pilot study. Skeletal Radiol 2004;33:277-282.
- Brown DE, James DC, Roy S. Pain relief by suprascapular nerve block in gleno-humeral arthritis. Scand J of Rheumatol 1988; 17:411-415.
- Feigl GC, Anderhuber F, Dorn C, et al: Modified lateral block of the suprascapular nerve: a safe approach and how much to inject? A morphological study. Reg Anesth Pain Med 2007;32:488-494.
- Peng P, Wiley MJ, Liang J, Bellingham G. Ultrasound-guided suprascapular nerve block: A correlation with fluoroscopic and cadaveric findings. Can J Anesth 2010;57:143-148.
- Mallon WJ, Brown HR, Vogler JB, Martinez S. Radiographic and geometric anatomy of the scapula. Clin Orthop Relat Res 1992; 277:142-154.
- Gofeld M. Ultrasonography in pain medicine: a critical review. Pain Pract 2008;8:226-240.
- Harmon D, Hearty C. Ultrasound-guided suprascapular nerve block technique. Pain Physician 2007;10:743-746.
- Yucesoy C, Akkaya T, Ozel O, et al. Ultrasonographic evaluation and morphometric measurements of the suprascapular notch. Surg Radiol Anat 2009;31:409-414.
- Smoljanovic T, Miklic D, Grgurevic L. Diameter of suprascapular nerve in the suprascapular notch. Pain Physician 2008;11:263-264.
Leave a commentOrder by
Newest on top Oldest on top