How I Do It: Obturator Nerve Block
Lower-extremity nerve block techniques such as the femoral nerve block, adductor canal block, and sciatic nerve block are regularly used to reduce pain and opioid consumption for lower-extremity procedures, but recent advancements in our understanding of lower-extremity anatomy paired with increased accessibility and quality of ultrasound equipment have led to both an explosion of novel techniques and renewed interest in older nerve blocks. The obturator nerve (ON) block, first described by Labat in 1922,[1] is finding its way back into the regular rotation. Thanks largely to the incredibly enlightening lower-extremity cadaveric dissection work done by Tran, Peng, and Short[2-4] and the emergence of the IPACK block,[5] the contributions of the ON and accessory obturator nerve to both hip and knee joints are becoming better understood.
Recent advancements in our understanding of lower-extremity anatomy paired with increased accessibility and quality of ultrasound equipment have led to both an explosion of novel techniques and renewed interest in older nerve blocks.
Although efficacious nerve block techniques for hip procedures may include the ON and accessory obturator nerve branches as parts of a collective target (eg, three-in-one block, suprainguinal fascia iliaca block, psoas compartment block, PENG block), study results recently demonstrated that a targeted ON block did not improve analgesia after total hip arthroplasty.[6] Because the ON block’s benefit is more established for proximal leg and knee procedures, we will limit discussion to that indication. The accessory obturator nerve will also be excluded because it seems to primarily innervate the anterior hip and has limited, if any, relation to the proximal leg and knee.
Anatomy
The ON originates in the lumbar plexus arising from the ventral rami of L2– L4. It has the most medial course of any branch in the lumbar plexus, descending medially along the psoas before exiting the obturator canal. It courses superficial to the obturator externus and deep to the pectineus muscle, where it typically bifurcates into an anterior and posterior division (Figure 1). Anagnostopoulou demonstrated considerable variability in where the division occurred in human dissections, noting 23% to be intrapelvic, 52% in the obturator canal, and 25% in the thigh.[7]
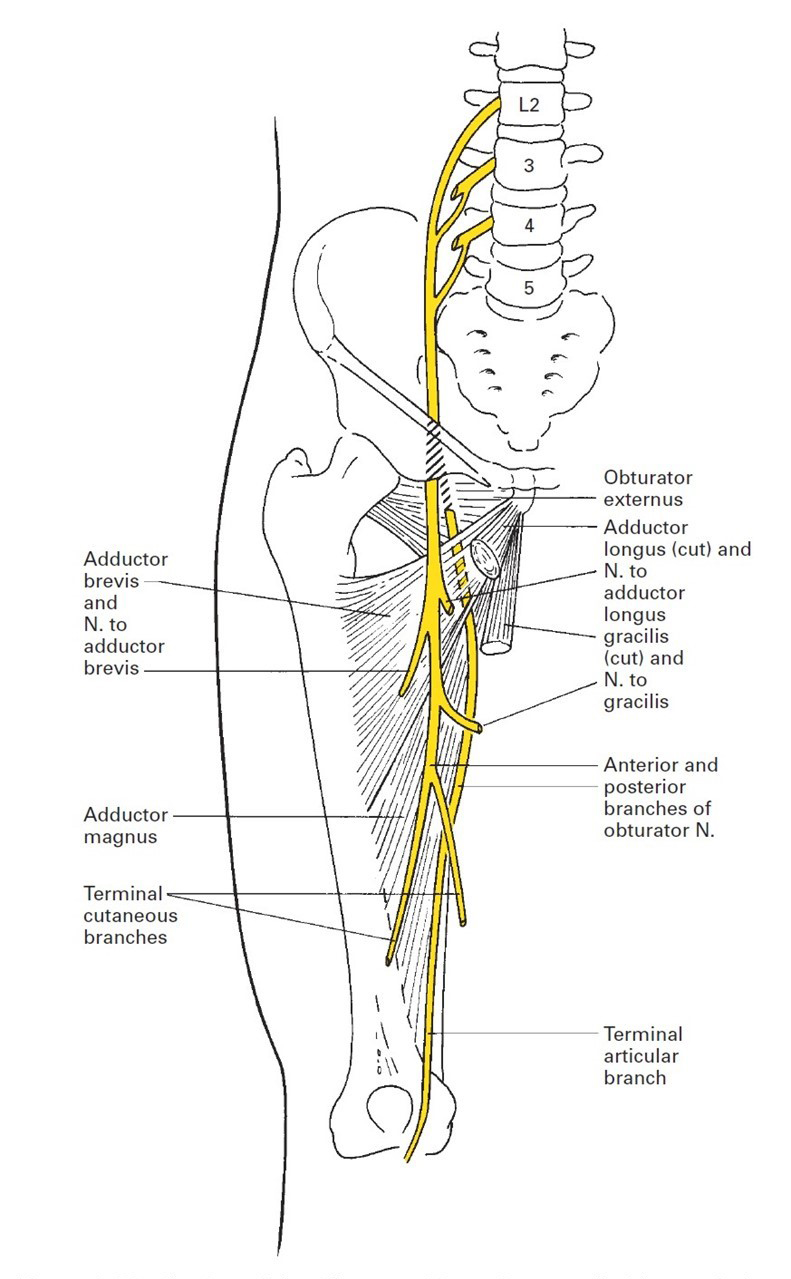
Figure 1: Distribution of the obturator nerve.
Reprinted with permission from Ellis H, Feldman S, Harrop-Griffiths W, Lawson A. Anatomy for Anaesthetists. 8th ed. Williston, VT. Blackwell Publishing. 2004.
After splitting, the anterior branch descends between the pectineus and adductor longus muscles whereas the posterior branch travels between the adductor longus and adductor brevis muscles. At the distal portion of the adductor longus, the anterior division can communicate with the saphenous nerve and may send branches to the medial thigh, and, in some dissections, articular branches to the medial knee.8 The posterior division will typically continue through the adductor hiatus and, combined with branches from the tibial nerve, gives rise to the popliteal plexus in the popliteal fossa.
Broadly, the ON contributes motor innervation to the leg adductor muscles, which, in addition to adducting the lower extremity at the hip joint, serve an important role in pelvic stability and balance during gait. The ON’s anterior branch typically supplies motor function to the adductor longus and gracilis muscles, whereas the posterior branch most often innervates the obturator externus and adductor magnus muscle (in conjunction with the tibial nerve). Both divisions innervate the adductor brevis muscle.[9]
Although the ON’s motor contribution is relatively consistent, its sensory innervation patterns are variable. Traditional dermatome maps suggest that the ON (via the anterior branch) is responsible for cutaneous innervation to the medial thigh, but Bouaziz et al found no discernable cutaneous distribution of blockade in more than half of 30 patients who underwent targeted ON block.[10]
The ON contributes anterior hip articular innervation via proximal intrapelvic and lower posterior branches.4 Articular innervation of the knee may arise from both branches, but the posterior is the most important contributor via the terminal articular branch from the popliteal plexus (Table 1). The terminal articular branch to the knee partially supplies the posterior articular capsule, cruciate ligaments, menisci, and synovial membrane of the knee,[9] but Gardner also described innervation to the anteromedial knee capsule.[11]
Table 1: Divisions of the obturator nerve with most common innervation patterns and relative indications for blockade
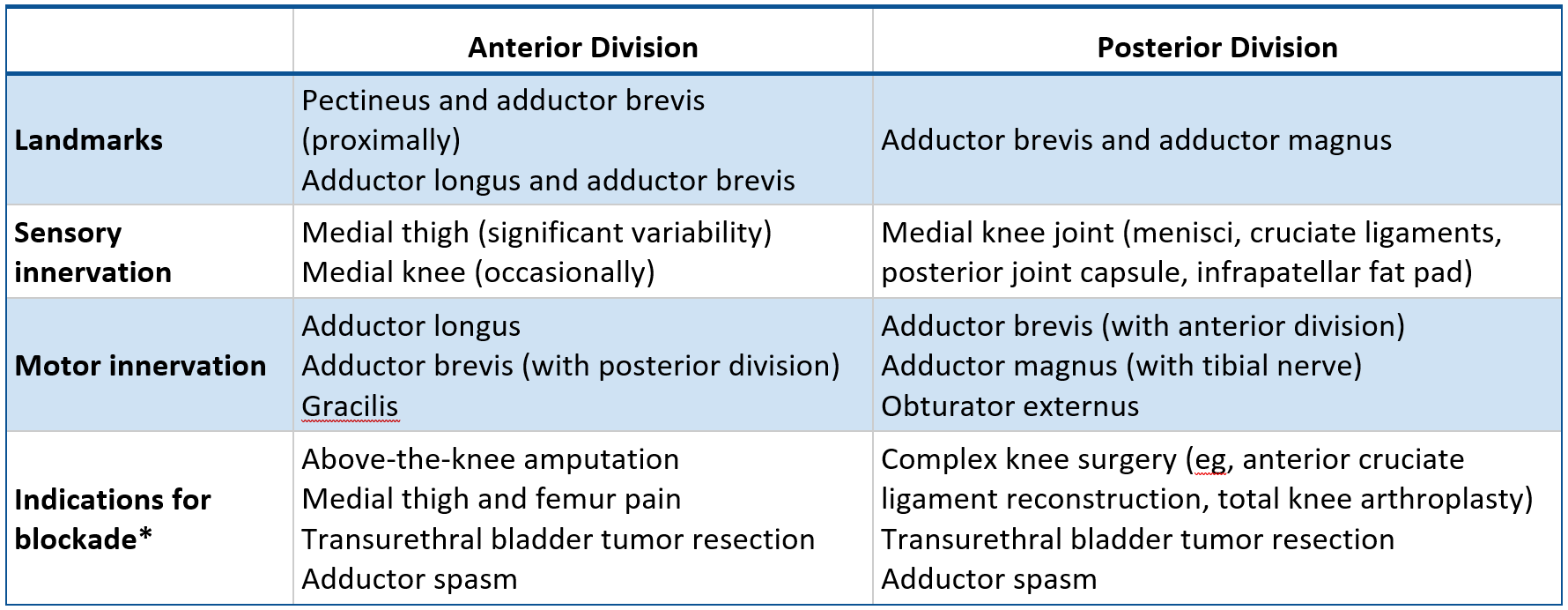
*Innervations are variable and overlap; in practice, both obturator nerve divisions are typically blocked in conjunction, but one division may be preferentially blocked or targeted with a higher volume when the indication requires.
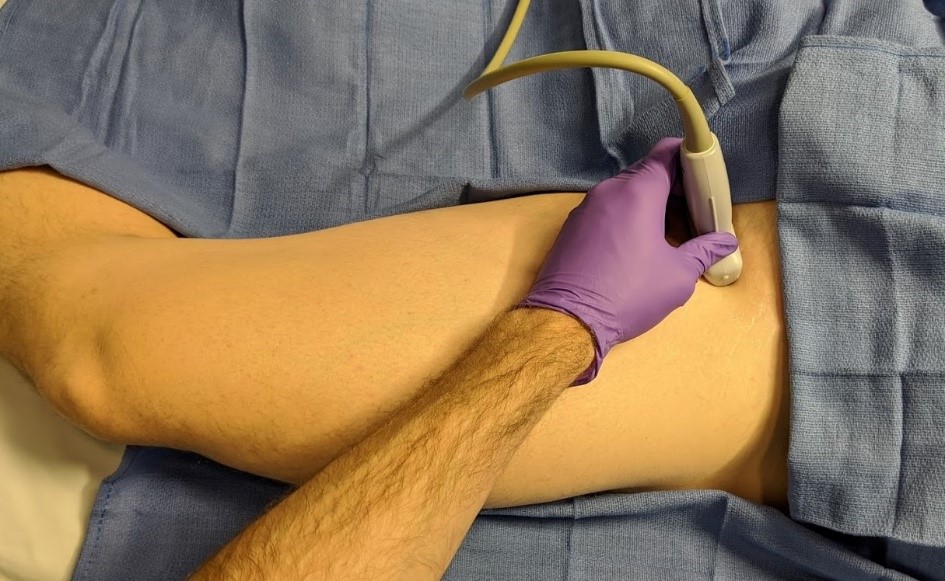

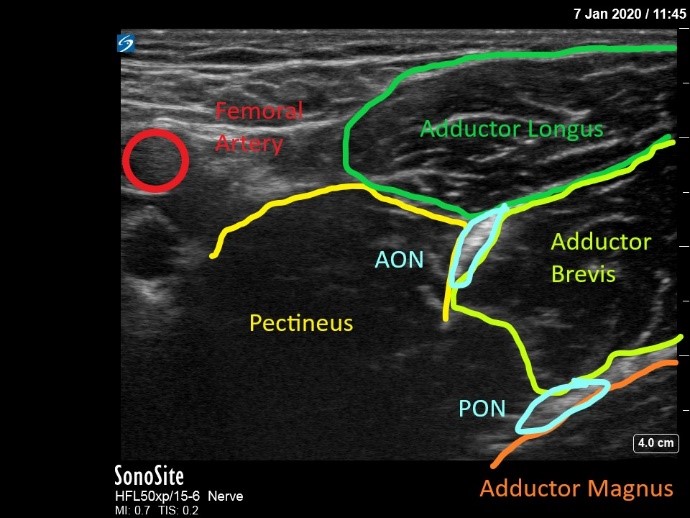
Figure 2: Distal approach the obturator nerve block with visualization of anterior and posterior divisions of the obturator nerve
AON, anterior division of obturator nerve; PON, posterior division of obturator nerve
Approach, Technique, and Positioning
Yoshida et al classified ON block approaches into two broad categories: distal and proximal.[12] The goal of a distal approach is to block the ON’s anterior and posterior divisions individually after they have bifurcated. Position the patient supine with the leg externally rotated and partially abducted. Align a linear ultrasound probe (preferably a high-frequency 10–15 MHz) parallel with the inguinal crease or alternatively 1–2 cm distal to the crease, perpendicular to the leg. First identify the femoral triangle, then move the probe medially to identify the adductor muscle group (Figure 2). Insert the needle in a lateral to medial direction, in plane with the ultrasound probe, advancing through the pectineus and toward the hyperechoic, interfascial structure (anterior division) that exists typically between the adductor brevis and adductor longus (sometimes visualized in a tricompartmental area with the pectineus). Use a nerve stimulator to confirm adductor twitch (typically 0.5–1.0 mA) if visualization is poor. Note that the neural stimulation of the adductor muscles by the anterior obturator nerve is more intense than the direct muscle stimulation that can be observed during advancement. After conf irming interfascial spread between the adductor longus and brevis, advance the needle toward the interfascial plane between the adductor brevis and magnus, where the posterior division resides. Target the individual branches selectively, if desired.
We prefer the distal approach and perform it almost exclusively when working with early trainees for a number of reasons. First, trainees tend to easily grasp new sonographic anatomy when it is presented in relation to adjacent anatomy they already understand (ie, the femoral triangle). Rarely do we perform an ON block without first performing a femoral nerve block via a fascia iliaca approach. Upon completion of a femoral nerve block, sliding the ultrasound probe medial in the same axial plane allows for immediate cross-sectional visualization of the pectineus, adductor longus, adductor brevis, and adductor magnus muscles. Second, the distal approach facilitates more consistent visualization and more predictable superficial anatomy. Trainees can struggle with finding the sonographic needle when probe tilt exceeds 10–15 degrees (cephalad tilting of 40–50 degrees can be required in proximal approaches), and the distal technique allows for a more neutral probe position. As they increasingly use various “plane” blocks (eg, transversus abdominis plane, quadratus lumborum, pectoralis nerve), trainees become accustomed to understanding the spread patterns associated with successful interfascial injections and therefore learn the ON block well when it is presented as an interfascial technique.


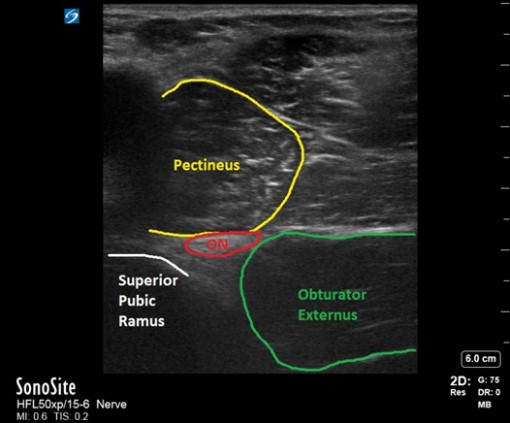
Figure 3: Proximal approach to the obturator nerve block as described by Lin.[17
ON, obturator nerve
Proximal techniques block the common ON with a single injectate of local anesthetic between the pectineus and obturator externus muscles. Although many proximal approaches have been described,[13-17] the approach by Taha[16] (and its subsequent modification by Lin[17]) is perhaps used most commonly. Patient positioning mirrors that of the distal approach. After aligning the probe along the inguinal crease and visualizing the adductor muscle group, tilt the probe cranially until the inferior margin of the superior pubic ramus is visualized in the medial field (Figure 3). Immediately lateral to the superior pubic ramus, visualize the pectineus (superficial) and obturator externus muscles (deep). Note that the superior pubic ramus is often aligned with the interfascial plane between the more superficial pectineus muscle and the obturator externus. Direct the needle in plane with the probe in a lateral to medial fashion. The hyperechoic ON can sometimes be directly visualized, but an interfascial injection is sufficient.
When working with a more advanced trainee (and when patient habitus allows), the proximal approach may be preferred because of its ability to block the common ON with a single injection. Although the ON can branch proximal to this level and the posterior division can pass through the obturator externus,[12] local anesthetic injection has been demonstrated to migrate proximally into the pelvis and reliably block both divisions.[15]
Indications
The inconsistencies of anatomic course and innervation patterns may account for the lack of consensus technique for ON blocks and more universal inclusion in analgesic plans. Perhaps the most accepted indication for ON block is as a component of a comprehensive analgesic and anesthetic plan for above-the-knee amputations. Interestingly, successful primary nerve block anesthetics for those amputations have been described with only femoral and sciatic nerve blocks, although increased sedation was required.[18] This may reflect the high variability in obturator innervation. Another common indication is anterior cruciate ligament reconstruction with gracilis tendon grafts.[19]
Outside of orthopedic procedures, an ON block may blunt adductor spasm during transurethral bladder tumor resections, and, according to one study by Tekgul et al, time to tumor recurrence may be improved by the addition of ON block.[20] The ON block has also been used to treat painful spasms with central nervous system pathologies such as multiple sclerosis, cerebral palsy, and paraplegia.[21]
The addition of a selective ON block to other established techniques has been shown to be of benefit in total knee arthroplasty (TKA), with Runge et al demonstrating that addition of an ON block to a femoral triangle block reduced opioid consumptions and pain scores when compared to femoral triangle block or local infiltration alone.[22-24] Despite demonstrable adductor weakness, the ability to ambulate postoperatively was not significantly worsened. Bendsten discussed the possibility of performing a targeted, posterior branch ON block in an effort to reduce adductor weakness, but it has not been reported to date.[25] Nonetheless, the threat of any impediments to early, aggressive rehabilitation postarthroplasty may be a barrier to using an ON block as part of any analgesic plan for TKA.
At our institution, ON blocks are performed for other indications, such as a variety of knee and leg procedures that involve instrumentation of the medial femur or medial femoral condyle, including femoral osteotomies to correct patellar tracking pathology, distal femoral fracture fixation, and complex multiligamentous knee reconstruction. On occasion, medial femur hardware removal may benefit from an ON block. It can also be used as a rescue block for a variety of knee procedures where preoperative femoral or adductor canal block in conjunction with infiltration between the popliteal artery and capsule of the posterior knee (IPACK) blocks are the core regional techniques.
Discussion
Broader use of ON block is limited by lack of consensus regarding approach, variability of the nerve’s anatomic course, concern for motor impact, and additional time and expertise required to perform an “extra” block. Additionally, like most regional techniques, sonographic resolution of the ON and its branches can be significantly limited by body habitus and muscle atrophy.
The approach of choice should be governed by your (and your trainee’s) comfort as well as clinical scenario. Although targeting the common obturator nerve with a single injection is ideal (and indeed has been successful in multiple described approaches), visualization and anatomic variability in common obturator nerve branch anatomy can make that challenging. On the other hand, sonographic visualization of approaches distal to the bifurcation may be easier to acquire but at the expenses of potentially higher volumes of injectate and increased procedure time. The distal approach does allow for targeting individual branches, which may prove to be useful. Your desired approach can also be thwarted by limitations in abduction and external rotation of the hip, resulting in suboptimal patient position. To date, we are aware of no studies comparing the analgesic efficacy of the two approaches.
Exercise additional caution when performing multiple nerve blocks for any procedure but specifically for above-the-knee amputations because the relatively larger doses of local anesthetic can be unsafe in a population already at elevated risk for local anesthetic toxicity, given their comorbidity burden and sometimes-advanced age. The medial thigh is a highly vascular area and vascular structures should be identified and avoided.[26] Venous structures can be especially challenging to identify in these planes, and unintended obturator vein puncture has been reported.[14]
Bendsten suggested the need for additional randomized control trials to further evaluate the efficacy of ON block for TKA.[25] Although the addition of an ON block may improve analgesia in TKA, no studies have compared targeted ON block to motor-sparing IPACK block. Although the addition of an ON block does not seem to affect ambulation post-TKA,[24] studies have not shown whether ON block increases fall risk. The degree of risk conferred by adductor motor weakness has not been quantified, nor has it been compared to the risks associated with systemic opioid administration. Further research is necessary to address these questions.
Case Study
One of the authors took it upon himself to experience an ON block (for science!) to better understand the sensations of adductor motor weakness and any cutaneous numbness. Under ultrasound guidance, a distal approach ON block was performed by depositing 10 mL of 2% chloroprocaine for each division of the obturator nerve, for a total of 20 mL. Within 10 minutes, he experienced adductor muscle weakness as an inability to forcibly adduct against even light resistance. He felt no appreciable sensory change in the anterior, medial, or posterior thigh or knee, despite testing with cold and sharp modalities. He had no noticeable deficit in ambulation. Adductor weakness resolved within roughly one hour. He tolerated the block overall, but when advancing the needle through the adductor longus en route to the interfascial plane where the posterior division of the ON was visualized, he reported moderate cramping and discomfort.
References
- Labat G. Regional Anesthesia: Its Technique and Clinical Application. Philadelphia, PA: Saunders; 1922.
- Tran J, Peng PWH, Gofeld M, et al. Anatomical study of the innervation of posterior knee joint capsule: implication for image-guided intervention. Reg Anesth Pain Med. 2019;44(2):234–238. https://doi.org/10.1136/rapm-2018-000015
- Tran J, Giron Arango L, Peng P, et al. Evaluation of the iPACK block injectate spread: a cadaveric study. Reg Anesth Pain Med. 2019;44(7):689–694. https://doi.org/10.1136/rapm-2018-100355
- Short AJ, Barnett JJG, Gofeld M, et al. Anatomic study of innervation of the anterior hip capsule: implication for image-guided intervention. Reg Anesth Pain Med. 2018;43(2):186–192. https://doi.org/10.1097/AAP.0000000000000701
- Sinha S. How I do it: infiltration between popliteal artery and capsule of knee (iPACK). ASRA News. February 2019. https://www. asra.com/asra-news/article/158/how-i-do-it-infiltration-between-poplite. Accessed February 11, 2020.
- Nielsen ND, Runge C, Clemmesen L, et al. An obturator nerve block does not alleviate postoperative pain after total hip arthroplasty: a randomized clinical trial. Reg Anesth Pain Med. 2019;44(4):466–471. https://doi.org/10.1136/rapm-2018-100104
- Anagnostopoulou S, Kostopanagiotou G, Paraskeuopoulos T, et al. Anatomic variations of the obturator nerve in the inguinal region: implications in conventional and ultrasound regional anesthesia techniques. Reg Anesth Pain Med. 2009;34(1):33–39. https://doi.org/10.1097/AAP.0b013e3181933b51
- Horner G, Dellon AL. Innervation of the human knee joint and implications for surgery. Clin Orthop Relat Res. 1994;301:221–226.
- Kumka M. Critical sites of entrapment of the posterior division of the obturator nerve: anatomical considerations. J Can Chiropr Assoc. 2010;54(1):33–42.
- Bouaziz H, Vial F, Jochum D, et al. An evaluation of the cutaneous distribution after obturator nerve block. Anesth Analg. 2002;94:445– 449. https://doi.org/10.1097/00000539-200202000-00041
- Gardner E. The innervation of the knee joint. Anat Rec. 1948;101(1):109–130. https://doi.org/10.1002/ar.1091010111
- Yoshida T, Nakamoto T, Kamibayashi T. Ultrasound-guided obturator nerve block: a focused review on anatomy and updated techniques. Biomed Res Int. 2017;7023750. https://doi.org/10.1155/2017/7023750
- Choquet O, Capdevila X, Bennourine K, et al. A new inguinal approach for the obturator nerve block: anatomical and randomized clinical studies. Anesthesiology. 2005;103(6):1238–1245. https://doi.org/10.1097/00000542-200512000-00020
- Akkaya T, Ozturk E, Comert A, et al. Ultrasound-guided obturator nerve block: a sonoanatomic study of a new methodologic approach. Anesth Analg. 2009;108(3):1037–1041. https://doi.org/10.1213/ane.0b013e3181966f03
- Yoshida T, Onishi T, Furutani K, Baba H. A new ultrasound-guided pubic approach for proximal obturator nerve block: clinical study and cadaver evaluation. Anaesthesia. 2016;71(3):291–297. https://doi.org/10.1111/anae.13336
- Taha, AM. Ultrasound-guided obturator nerve block: a proximal interfascial technique. Anesth Analg. 2012;114(1):236–239.
- Lin JA, Nakamoto T, Yeh SD. Ultrasound standard for obturator nerve block: the modified Taha’s approach. Br J Anaesth. 2015;114(2):337–339. https://doi.org/10.1093/bja/aeu467
- Chandran R, Beh ZY, Tsai FC, Kuruppu SD, Lim JY. Peripheral nerve blocks for above knee amputation in high-risk patients. J Anaesthesiol Clin Pharmacol. 2018;34(4):458–464. https://doi.org/10.4103/joacp.JOACP_346_17
- Sakura S, Hara K, Ota J, Tadenuma S. Ultrasound-guided peripheral nerve blocks for anterior cruciate ligament reconstruction: effect of obturator nerve block during and after surgery. J Anesth. 2010;24(3):411–417. https://doi.org/10.1007/s00540-010-0916-3
- Tekgul Z, Divrik R, Turan M, Konyalioglu E, Simsek E, Gonullu M. Impact of obturator nerve block on the short-term recurrence of superficial bladder tumors on the lateral wall. Urological Onc. 2014;11(1):1248–1252. https://doi.org/10.22037/uj.v11i1.1819
- Lam K, Wong D, Tam CK, et al. Ultrasound and electrical stimulator-guided obturator nerve block with phenol in the treatment of hip adductor spasticity in long-term care patients: a randomized, triple blind, placebo controlled study. J Amer Med Direc Assoc. 2015;16(3):238–246. https://doi.org/10.1016/j.jamda.2014.10.005
- Sato K, Sai S, Shirai N, Adachi T. Ultrasound guided obturator versus sciatic nerve block in addition to continuous femoral nerve block for analgesia after total knee arthroplasty. Jpn Clin Med. 2011;2:29–34. https://doi.org/10.4137/JCM.S7399
- Macalou D, Trueck S, Meuret P, et al. Postoperative analgesia after total knee replacement: the effect of an obturator nerve block added to the femoral 3-in-1 nerve block. Anesth Analg. 2004;99(1):251– 254. https://doi.org/10.1213/01.ane.0000121350.09915.84
- Runge C, Børglum J, Jensen JM, et al. The analgesic effect of obturator nerve block added to a femoral triangle block after total knee arthroplasty: a randomized controlled trial. Reg Anesth Pain Med. 2016;41(4):445–451. https://doi.org/10.1097/AAP.0000000000000406
- Bendtsen TF, Moriggl B, Chan V, Børglum J. The optimal analgesic block for total knee arthroplasty. Reg Anesth Pain Med. 2016;41(6):711–719. https://doi.org/10.1097/AAP.0000000000000485
- Paraskeuopoulos T, Saranteas T. Ultrasound-guided obturator nerve block: the importance of the medial circumflex femoral vessels. Reg Anesth Pain Med. 2012;37(5):565. https://doi.org/10.1097/AAP.0b013e318260e712
Leave a commentOrder by
Newest on top Oldest on top