President’s Message: ASRA Pain Medicine: The Gold Standard in Guidelines and Education
Cite as: Provenzano D. President’s message: ASRA Pain Medicine, the gold standard in guidelines and education. ASRA Pain Medicine News 2025;50. https://doi.org/10.52211/asra020125.001.
President’s Message
 In 2006 I graduated from my chronic pain fellowship at Dartmouth Hitchcock Medical Center in New Hampshire. The training that I received was amazing and provided me with a strong foundation to enter the “real world”
of practicing pain medicine. During my time in New Hampshire, I had a great mentorship and developed lasting friendships.
In 2006 I graduated from my chronic pain fellowship at Dartmouth Hitchcock Medical Center in New Hampshire. The training that I received was amazing and provided me with a strong foundation to enter the “real world”
of practicing pain medicine. During my time in New Hampshire, I had a great mentorship and developed lasting friendships.
While I was there, I did not realize that some of these friendships would further blossom in my new postgraduate academic home, ASRA Pain Medicine. One of these friendships that was initiated and continues today is with Dr. Brian Sites. Early in my training and fellowship, Dr. Sites was an attending in the department of anesthesiology and occasionally assisted the chronic pain department with epidural steroid injections. Some of my first interlaminar epidural steroid injections were performed with Dr. Sites as the supervising physician. It is amazing to reflect on how, over the course of almost 20 years, Dr. Sites and I grew up in ASRA Pain Medicine and eventually took leadership positions for the society. Dr. Sites was a previous board member and now is the editor-in-chief of our prestigious journal, Regional Anesthesia & Pain Medicine.

I also had the pleasure of meeting Dr. Alexios Carayannopoulos, who was in the fellows class the following year and led the 22nd Annual ASRA Pain Medicine Meeting.

I began my first job in the fall of 2006. Like all new graduates, I faced daily challenges, including managing a complex medical condition that is often not cured and navigating a flawed healthcare system. In the spring of 2007, I read Dr. B. Todd Sitzman’s president’s message for the American Academy of Pain Medicine titled, “Guiding Principles for the Pain Medicine Physician – in a Not so Ideal World.” Though I didn’t know Dr. Sitzman, his message resonated with me, and I pinned it on my office bulletin board. Dr. Sitzman described an ideal world in pain medicine:
- Correct diagnosis on the first visit
- High patient compliance and response rates
- Limited need for follow-up care due to full recovery
- Adequate reimbursement without bureaucratic challenges
- No addiction to prescribed analgesics1
The message gave me insight and reassured me that I was not the only one who was not practicing in an “ideal world.” One of my greatest joys and benefits of volunteering in organized medicine is the friendships I have formed. It’s ironic that Todd and I became great friends years later through our work with the North American Neuromodulation Society and teaching at ASRA Pain Medicine. Both Todd and I manage busy private practices. We also understood the importance of academic work and finding the time to contribute and volunteer to improve the practice of pain medicine.

In 2025, the “ideal world” still does not exist. Reflecting on the 23rd Annual Pain Medicine Meeting and future goals for 2025, I recognized how ASRA Pain Medicine has enhanced my clinical skills and its crucial role in fostering ethical and effective practices in pain medicine. This encompasses delivering high-quality care and participating and surviving in a healthcare system that frequently undervalues physicians’ contributions. The education and member services ASRA Pain Medicine provided have enabled me to excel in this challenging world. Below, I will provide insights and updates on the 23rd Annual Pain Medicine Meeting, 50th Annual Regional Anesthesiology and Acute Pain Medicine Meeting, and future educational offerings for 2025.
The 23rd Annual Pain Medicine Meeting was a huge success under the leadership of Dr. Christine Hunt. The attendance was phenomenal, and the number of abstracts submitted and presented was record-breaking (513 submitted abstracts). This record-breaking number of abstracts highlights the importance of research and fostering its development and communication with ASRA Pain Medicine members. I am extremely thankful to all the researchers and committee members who have allowed the review and dissemination of this important science to our members. Furthermore, as a reminder, ASRA Pain Medicine continues to fund research substantially through its annual research grants and awards. The next Call for Letters of Intent will take place in July 2025. The Fall Meeting covered key topics in pain medicine, including optimal pain practices, interventional anatomy, best practices for radiofrequency ablation, complex regional pain syndrome challenges and treatment strategies, the connection between pain and health span (eg, aging, nutrition, and lifestyle medicine), best spine care practices, buprenorphine, naloxone and naltrexone for chronic pain management, and advanced neuromodulation techniques for pain and other conditions. Each session provided tips on billing and coding for ethical and cost-effective treatment implementation. For example, Dr. Trent Emerick discussed G code G2211 for reimbursing longitudinal care relevant to pain medicine (a supplemental article on G2211 can be found here). In addition, Dr. Aaron Calodney explained billing for sacroiliac joint fusions.
We also need to prepare residents and fellows for their entrance into the real world. The Fall Meeting and its associated activities highlighted the emphasis on solidifying and supporting our relationships with program directors, offering significant educational opportunities to fellows, and enhancing relationships and collaborations among young physicians with each other and mentors. It was a joy to meet in person with the leadership of the Association of Pain Program Directors, including Drs. Meredith Barad, Alexander Bautista, Lynn Kohan, and Trent Emerick.

We brainstormed about the needs of fellows and program directors and ensured ASRA Pain Medicine’s continued support and partnership in their mission. We made it clear that we would not degrade or undermine the current state of fellowship training as we have recently seen in social media and publications, but rather, we would help it flourish. Remember, it is unrealistic to learn everything in 12 months that you will need for your future career. The practice of medicine requires continuous learning.
As Sir William Osler said at McGill University in 1905, “The hardest conviction to get in the mind of a beginner is that the education upon which he is engaged is not a college course, not a medical course, but a life course, for which the work of a few years under teachers is but preparation.”
The main goal of the fellowship is to provide a strong foundation for future pain medicine doctors to enter the world and provide high-quality care. ASRA Pain Medicine will continue to provide the learning and mentorship that future physicians need. The Advanced Interventional Pain Management Course and Workshop for Fellows was held for the second time in conjunction with the 23rd Annual Pain Medicine Meeting. This exclusive event covered the most relevant and popular topics in pain practice with didactic and cadaveric sessions throughout the day. The fellows who participated gave great feedback:
- “Amazing course for any pain medicine fellow. We learned from the most knowledgeable faculty and true experts in the field! What a privilege to be able to attend this course.”
- “The fellows course was excellent. A great opportunity to learn from the field’s experts.”

The Fall Meeting featured several sessions throughout the 3 days specifically for residents and fellows from perspectives on applying to fellowship to practice management roundtable discussions. There were also opportunities for networking and fun with the Resident/Fellow and Program Director Meet and Greet and the Resident & Fellow Committee Quiz Bowl.

Dr. Donald Arnold, the current president of the American Society of Anesthesiologists (ASA), also attended our Fall Meeting, and we had great discussions with him regarding the pain specialty and our future collaboration to provide postgraduate training on advanced pain techniques by combining our educational offerings.

Thank you to all those who attended the Fall Meeting and our industry supporters. I truly hope you enjoyed the Fall Meeting as much as I did and that you gained significant information that allowed you to improve your practice when you returned home. I found the content helpful in succeeding in the less than "ideal world.”
In the spring in Orlando, Florida, Dr. Vishal Uppal will lead the 50th Annual Regional Anesthesiology and Acute Pain Medicine Meeting, focusing on safety, efficacy, and innovation. This meeting will feature a comprehensive scientific program addressing critical topics in regional anesthesia and acute pain medicine (RAAPM), including a special lecture by Dr. Anand Rao on artificial intelligence in healthcare.
Key topics will include point-of-care ultrasound with an emphasis on GLP-1 agonist drugs and the significance of gastric ultrasound interpretation, updates from sister societies (ESRA, LASRA, AFSRA, and AOSRA-PM), perioperative pain management for individuals with complex regional pain syndrome, the role of neurostimulation in acute pain management, and regional anesthesia safety. Additionally, more than 40 problem-based learning discussions will cover subjects such as acute pain and regional care for hip and rib fractures, methods to optimize epidural analgesia, practices to reduce the environmental impact of anesthetic practice, and techniques to enhance scientific writing. The event will also feature notable social gatherings, including the Jubilee Gala. This meeting promises to be extraordinary, showcasing the history of and future outlook for acute pain and regional anesthesia care. In the short video below, Dr. Uppal shares additional highlights for this anniversary meeting.
This meeting is also an opportunity to meet with the Regional Anesthesiology Fellowship Directors Association (RAFDA) leadership and learn how we can best support them and their fellows. For over two decades, this has been a voluntary group primarily composed of fellowship directors in North America, working collaboratively on initiatives to improve the training experience. Members of this group have been instrumental in codifying educational standards, obtaining Accreditation Council for Graduate Medical Education accreditation for the subspecialty, and moving to a formalized match process. We will continue to work with the RAFDA to promote RAAPM fellowship training and provide additional resources to help the subspecialty flourish.
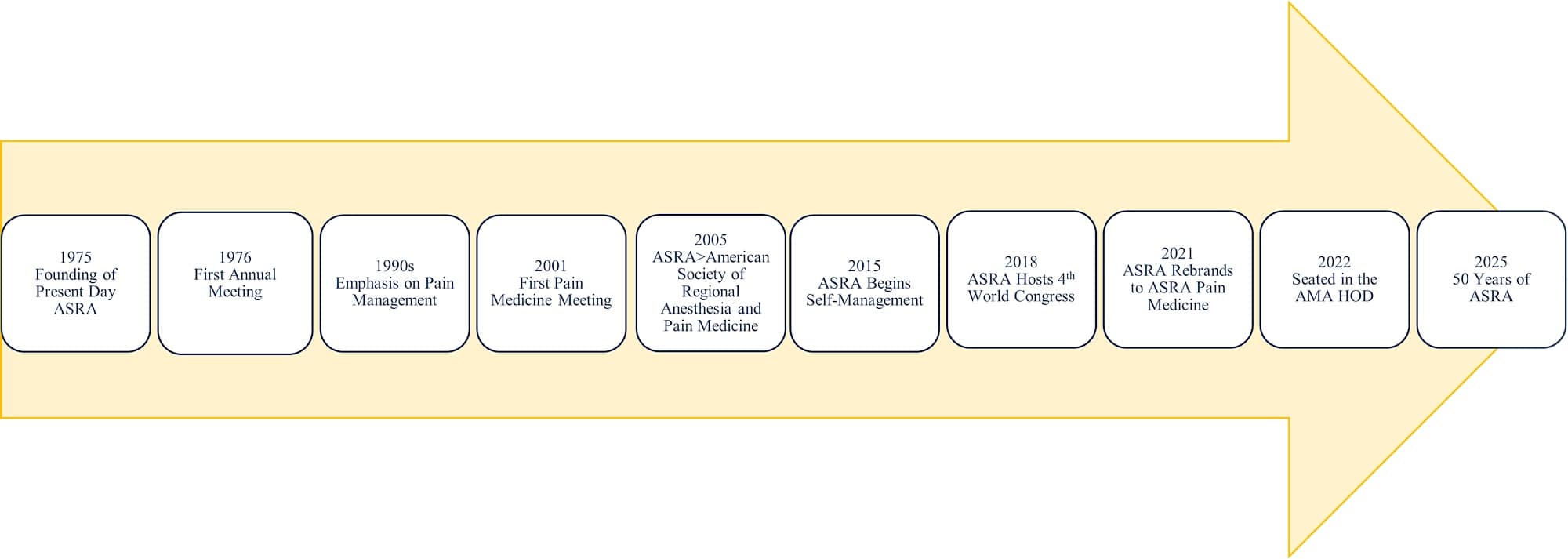
Reflecting on the society’s growth during the past 50 years, it is important to acknowledge the contributions of dedicated volunteers. None of this would have been possible without the strength of the volunteers at ASRA Pain Medicine. I am truly grateful for all the volunteers’ time, expertise, and unwavering support of the society’s mission and vision. It’s amazing to see the great strides made in 50 years.
To prosper in this less than “ideal world,” continued education from an organization with a strong research, education, and advocacy foundation is needed. In addition, the messaging and education must be of the highest quality. Hence, it continues to be respected and valued by all healthcare community members, including physicians, practice managers, government agencies, and insurance companies. ASRA Pain Medicine has been around for over 50 years. It will continue to flourish and offer high-quality educational content that can be used for the growth of an individual physician in the field of pain medicine. We are excited to launch our new webinar series under Dr. Raj Gupta, which will cover such topics as post-dural puncture headache, cannabis and surgery, and perioperative management for spinal cord stimulation in chronic non-cancer pain, and our new learning management system under the guidance of Dr. Stuart Grant. Both these resources will allow for education outside of in-person meetings.
In addition, we recently released two guidelines that will enhance patient safety. The ASRA Pain Medicine Consensus Practice Infection Control Guidelines for Regional Anesthesia and Pain Medicine are designed to minimize infections in patients undergoing surgery. Surgical site infections are the second most reported healthcare-related infection in the United States. Unfortunately, recent data from the Centers for Disease Control from 2022 demonstrated that infection rates continue to increase, showing a 4% increase in the standardized infection ratio related to the National Healthcare Safety Network operative procedures categories combined with the previous year. Implantable device infections are also associated with significant costs, legal implications, and, most importantly, patient morbidity and mortality.2-6 The second guideline on performing regional anesthetic techniques in patients receiving antithrombotic or thrombolytic therapy was led by Dr. Sandy Kopp. Dr. Kopp briefly details the history and the updates to these guidelines below.
The development and evolving status of standards for the prevention of perioperative venous thromboembolism, as well as the introduction of increasingly more potent antithrombotic medications, resulted in concerns regarding the heightened risk of neuraxial bleeding after neuraxial and deep plexus or deep peripheral blocks. In response to these ongoing patient safety issues, the American Society of Regional Anesthesia and Pain Medicine (ASRA Pain Medicine) has published four previous sets of evidence-based recommendations for managing regional anesthesia in patients receiving antithrombotic or thrombolytic therapy. The 1998 and 2003 editions focused on neuraxial blocks and anticoagulants in surgical patients, while the 2010 publication also addressed, for the first time, the risk of significant bleeding in patients undergoing plexus and peripheral techniques. The fourth edition, published in 2018, included a comprehensive review of the management of thromboprophylaxis in the parturient and acknowledged the need for separate recommendations for patients undergoing interventional pain procedures while receiving antithrombotic therapy.
The fifth edition of the American Society of Regional Anesthesia and Pain Medicine’s Evidence-Based Guidelines on Regional Anesthesia in Patients Receiving Antithrombotic or Thrombolytic Therapy reviews the published evidence since 2018. It provides guidance to help avoid this rare but potentially catastrophic complication. It is impossible to perform large, randomized controlled trials evaluating a complication this rare; therefore, where the evidence is limited, the authors continue to maintain an antihemorrhagic approach focused on patient safety and have proposed conservative times for the interruption of therapy prior to neural blockade. In previous versions, the anticoagulant doses were described as prophylactic and therapeutic. In this version, we will be using low dose and high dose, which will allow us to be consistent with other published guidelines and more accurately describe the dose in the setting of specific patient characteristics and indications. Due to the increasing ability to obtain drug-specific assays, we have included suggestions for when ordering these tests may be helpful and guide practice. Like previous editions, at the end of each recommendation, the authors clearly noted how the recommendation had changed from previous editions.
Both guidelines are extremely important to the field of pain medicine, and we are grateful to everyone who contributed.
At the recent ASRA Pain Medicine Meeting, Dr. Samer Narouze gave an excellent talk on the history of pain medicine, discussing its successes and challenges. Looking back on history, we can learn a lot, including how some previous technologies we introduced are no longer covered or utilized. The future of pain medicine is bright, but we can learn from history, which demonstrates that when there is less than ideal research, overutilization, and indiscriminate deployment of therapies, the field is set back. One of the main reasons that I have decided to dedicate most of my volunteer time to ASRA Pain Medicine is because I have truly found a home where evidence-based pain medicine is taught, preserved, and refined by a very solid group of physicians, who are committed to an organization with a long history and future lifeline.
In conclusion, 2024 was a notable year for ASRA Pain Medicine. Looking forward, 2025 holds potential for further advancements as we continue to focus on pain medicine education and research. Additionally, we aim to reduce bureaucratic and financial barriers through our advocacy efforts in collaboration with the American Medical Association, the Pain Medicine Coalition with ASA and the International Pain and Spine Intervention Society, and our industry partners. Thank you for your dedication and membership. Your dues support our mission; the $410 spent on renewal contributes to these causes. I believe it is money well spent; I hope you do too.
References
- Sitzman BT. Guiding principles for the pain medicine physician--in a not-so-ideal world. Pain Med2007;8(4):293-4. https://doi.org/10.1111/j.1526-4637.2007.00322.x
- Perencevich EN, Sands KE, Cosgrove SE, et al. Health and economic impact of surgical site infections diagnosed after hospital discharge. Emerg Infect Dis 2003;9(2):196-203. https://doi.org/10.3201/eid0902.020232
- National Healthcare Safety Network. Surgical site infection (SSI) event. Centers for Disease Control and Prevention. https://www.cdc.gov/nhsn/pdfs/pscmanual/9pscssicurrent.pdf. Published January 2025. Accessed January 27, 2025.
- Fitzgibbon DR, Stephens LS, Posner KL, et al. Injury and liability associated with implantable devices for chronic pain. Anesthesiology 2016;124(6):1384-93. https://doi.org/10.1097/ALN.0000000000001122
- O’Brien WJ, Gupta K, Itani KMF. Association of postoperative infection with risk of long-term infection and mortality JAMA Surg 2019;155(1):61-8. https://doi.org/10.1001/jamasurg.2019.4539
- Goel V, Kumar V, Agrawal SN, et al. Outcomes associated with infection of chronic pain spinal implantable electronic devices: insights from a nationwide inpatient sample study. Neuromodulation 2021;24(1):126-34. https://doi.org/10.1111/ner.13263