How I Do It
Learn from your colleagues. ASRA Pain Medicine members share how they perform common procedures and accomplish other tasks.
- Listed by publication date, most recent on top
How I Do It: Infiltration Between Popliteal Artery and Capsule of Knee (iPACK)
Introduction
Controlling posterior knee pain after total knee arthroplasty is an important component of the comprehensive strategy for providing postoperative analgesia. This pain is mediated by articular branches that originate primarily from the tibial component of the sciatic nerve with contributions from the obturator nerve (Figure 1) [1],[2]. Posterior knee pain can be controlled by sciatic nerve block, but leads to undesirable foot drop and may delay diagnosis and treatment of surgically induced common peroneal nerve injury. A selective tibial nerve block in the popliteal fossa is an alternative to sciatic nerve block and can provide analgesia without causing a foot drop, but it decreases sensory perception in the sole of the foot and causes weakness of plantar flexion [3].
The goal of iPACK is to selectively block only the innervation of the posterior knee joint while sparing the main trunks of tibial and common peroneal nerves, thereby maintaining the sensorimotor function of the leg and foot.
The articular branches, after arising from the main trunks of the tibial and obturator nerves, travel through a tissue space between the popliteal artery and the femur to innervate the posterior capsule of the knee (Figure 2). These articular branches can be blocked by infiltrating this tissue plane between the popliteal artery and the capsule of the knee (iPACK) with local anesthetic solution under ultrasound guidance. The goal of iPACK is to selectively block only the innervation of the posterior knee joint while sparing the main trunks of tibial and common peroneal nerves, thereby, maintaining the sensorimotor function of the leg/foot. We introduced the iPACK technique at the American Society of Regional Anesthesia (ASRA), Spring meeting in 2012 [4].
Technique: The Early Years
When we conceived the concept of iPACK, our injections were performed with the patient in a prone position. Even though we have since transitioned to performing the iPACK in a supine position, it is still worthwhile to review the original injection technique to get a better understanding of the sonoanatomy and procedure.
Sonoanatomy
With the patient in a prone position, a high frequency linear probe or the low frequency curvilinear transducer can be used depending on body habitus. Another advantage of the curvilinear probe is the wide scanning view. The probe is placed transversely at or just above the popliteal crease to visualize the femoral condyles and the popliteal artery in cross-section (Figure 3). At this level, the femoral condyles appear as discontinuous, curved hyper-echoic lines. The popliteal artery is seen as a pulsating anechoic structure in the center of the scan. The popliteal vein may be compressed from pressure of the transducer and not be visible on the image.
From this point, the probe is moved cephalad, keeping the popliteal artery in view, till the discontinuous, interrupted hyperechoic line of the condyles changes to a continuous, hyper-echoic silhouette of the femoral shaft just cranial to the condyles. The location of the tibial nerve (superficial to popliteal artery) and the common peroneal nerve (lateral edge of sonogram) can be seen by changing the tilt of the transducer. The plane between the popliteal artery and the femur is the space through which the articular branches are traversing and is the target tissue space for infiltration.
Needle Insertion Technique
The needle is inserted via an in-plane, medial to lateral approach. The insertion point is parallel to the femur, in the middle of the tissue plane. The needle is advanced till the needle tip is positioned 2 cm beyond the lateral border of the popliteal artery. Subsequently, the local solution is injected in 3 ml aliquots as the needle is withdrawn. Injecting the local as the needle is being withdrawn ensures even spread of local solution. Typically, 20 mL (range of 15 -25 mL) of local solution is infiltrated in the tissue plane. Ropivacaine 0.2% or Bupivacaine 0.25% with epinephrine 1:200,000 can be used for iPACK.
With the scanning procedure described above, the image required for iPACK can be developed with patient in supine (knee flexed or extended) or lateral decubitus positions. We recommend that the needle should be inserted in a medial to lateral direction and the needle tip not be pushed 2 cm beyond the lateral edge of the popliteal artery to avoid anesthetizing the common peroneal nerve and causing a foot-drop. If a lateral decubitus position is used, the side to be injected should be dependent, so that needle can be inserted from the medial thigh.
Current Technique
Over time our technique has evolved to performing the iPACK injection with the patient supine and scanning from a posteromedial acoustic window. Since iPACK is usually combined with adductor canal block or femoral nerve block, our current technique avoids multiple prepping or draping and position changes for different blocks.
The patient is placed in a supine position with the lower extremity flexed at the knee and abducted at the hip (frog leg position). A roll of blanket is placed under the thigh to support it (Figure 4). To begin scanning, the transducer is placed on the lower third of the medial thigh to visualize the femur and the femoral vessels in cross-section. The transducer is then slid caudally observing the femoral artery as it dives into the popliteal fossa through the adductor hiatus to become the popliteal artery. At this point, the transducer is moved posteriorly and inferiorly to visualize the space between the popliteal artery and the shaft of the femur just superior to the femoral condyles. The needle is inserted, in plane, from the anterior end of the transducer in a medial to lateral trajectory, keeping the needle parallel to the acoustic shadow of the femur. With the needle tip resting 2 cm beyond the lateral border of the artery, 20 mL of local anesthetic solution is injected, after negative aspiration of blood, to infiltrate the tissue space in divided doses as the needle is withdrawn. The local anesthetic injectate is a mixture of 15mL of Bupivacaine 0.25% combined with 5mL of liposomal bupivacaine 1.3%.
In our practice, iPACK has largely replaced selective tibial nerve block as part of the multi-modal regimen for controlling posterior knee pain after total knee arthroplasty and cruciate ligament surgeries. Future studies should be undertaken to further refine the technique.
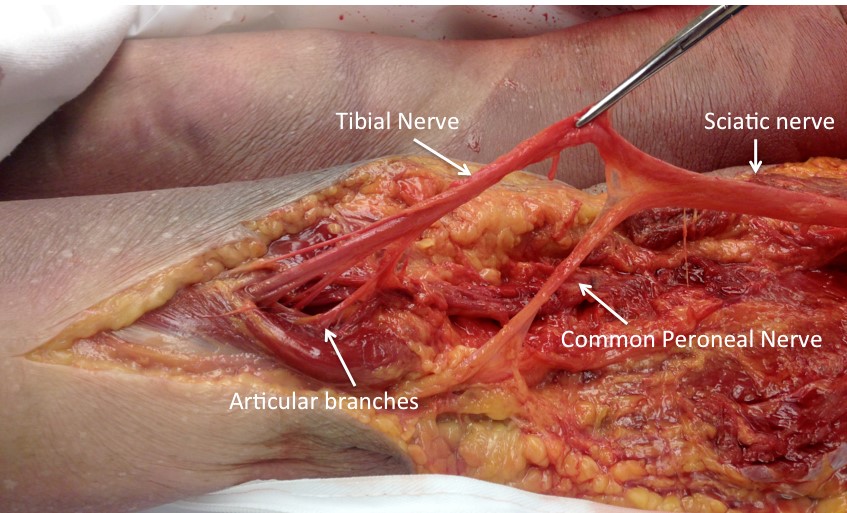
Figure 1: Dissection of Popliteal Fossa Showing Articular Branches to Posterior Knee Arising From Tibial Nerve
(Image courtesy of the Department of Anatomy at Penn State College of Medicine, State College, PA)
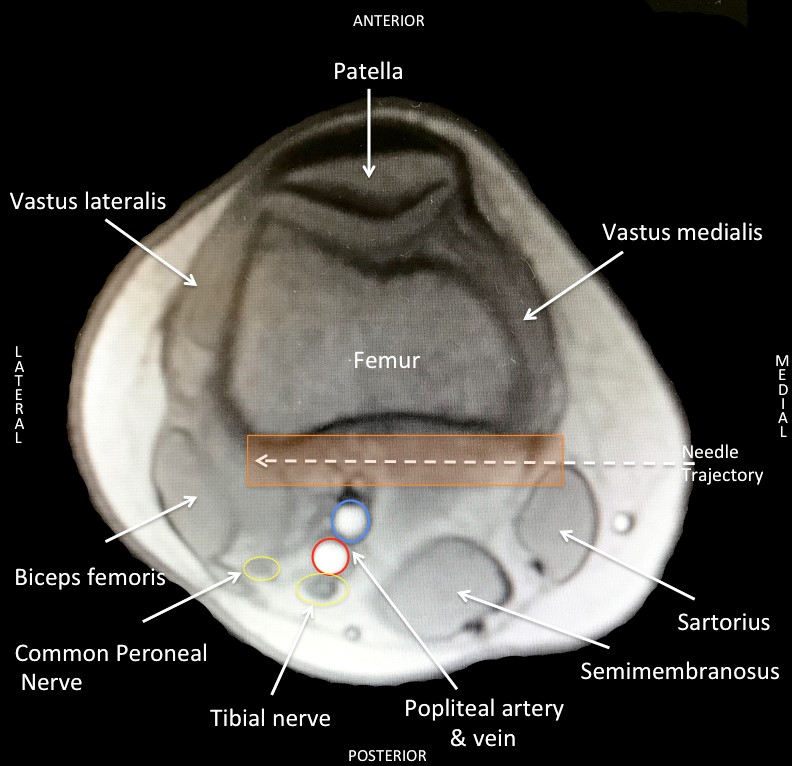
Figure 2: Cross-Sectional Anatomy of Thigh Proximal to Femoral Condyles
Orange box = target tissue plane for iPACK injection
(Image courtesy of the author)
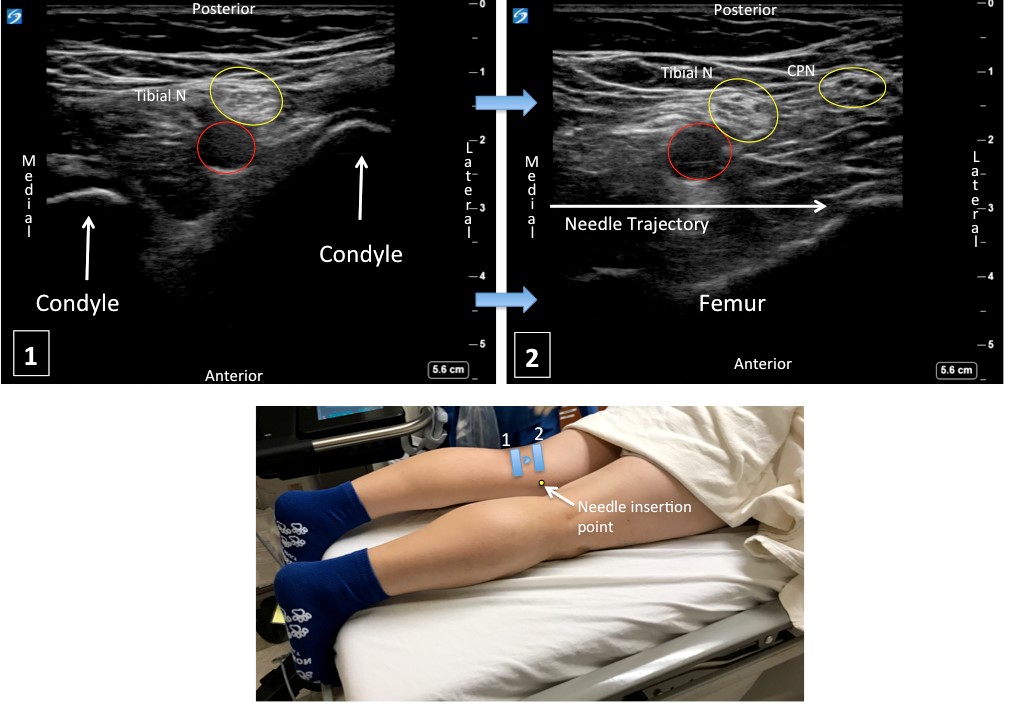
Figure 3: Scanning Sequence of Popliteal Fossa for iPACK With Corresponding Sonograms
Red circle = popliteal artery
(Image courtesy of the author)
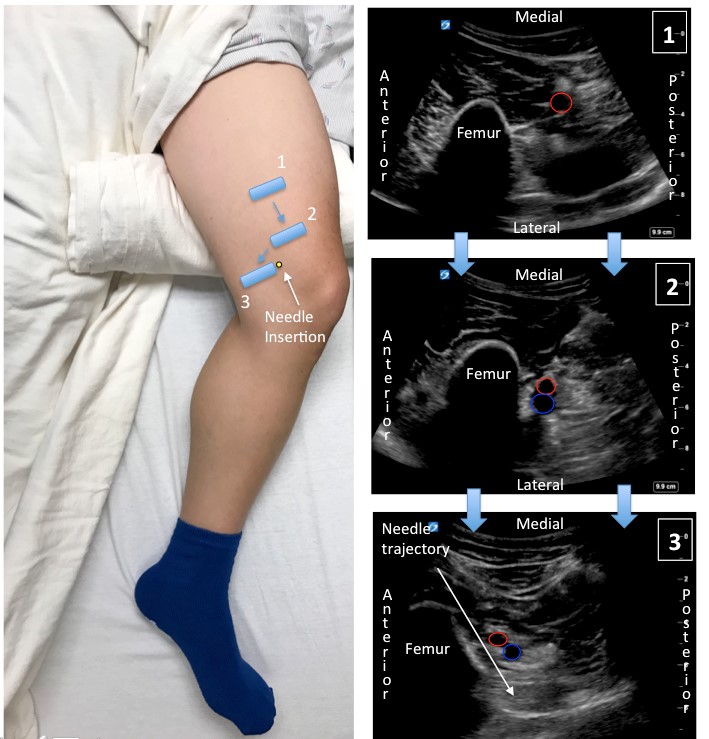
Figure 4. Scanning Sequence for iPACK Using the Posteromedial Acoustic Window With Corresponding Sonograms
Red circle = popliteal artery; blue circle = popliteal vein
References:
- Gardner E. The innervation of the knee joint. Anat Rec. 1948;101:109–130.
- Horner G, Dellon AL. Innervation of the human knee joint and implications for surgery. Clin Orthop Relat Res. 1994; 301:221–226.
- Sinha SK, Abrams JH, Arumugam S, et al. Femoral nerve block with selective tibial nerve block provides effective analgesia without foot drop after total knee arthroplasty: a prospective, randomized, observer-blinded study. Anesth Analg. 2012;115:202–206. https://doi.org/10.1213/ANE.0b013e3182536193
- Sinha S, Abrams J, Sivasenthil S, et al. Use of ultrasound guided popliteal fossa infiltration to control pain after total knee arthroplasty: a prospective, randomized, observer-blinded study (Abstract P 52). Presented at: American Society of Regional Anesthesia (ASRA) Meeting, March 2012; San Diego, CA.
Leave a commentOrder by
Newest on top Oldest on top