View by publication date
(most recent on top)
Latest articles
How I Do It: Transversus Thoracic Plane Block
The opioid crisis currently threatening the health of the global population has compelled health care providers to reconsider appropriate analgesic options. Massive efforts have been made to maximize multimodal analgesia and regional anesthetic techniques in an attempt to reduce pain and the need for opioid analgesics. These efforts have been associated with improvements in ultrasound imaging technology and a renewed interest in anatomical study that has resulted in a proliferation of fascial plane blocks to assist in the provision of perioperative analgesia.
Although the notion of pain as the fifth vital sign now appears misguided, postsurgical pain continues to limit recovery and may increase the risk of perioperative morbidity. Poorly managed chest wall pain can contribute to an increased incidence of pulmonary complications through increased splinting. Restricted postoperative breathing can result in hypoventilation, atelectasis, pneumonia, and an increased length of hospital stay. Thus, treating surgical chest pain adequately and in a manner that minimizes the requirement for significant opioid administration is important.
Midline chest wall pain can be iatrogenic from median sternotomy and pacemaker placement, or pathologic from sternal and medial rib fractures. Chronic pain can develop following poor management of acute pain, contributing to additional physiologic and psychologic stress and consuming disproportionate physical and financial resources.
Treating surgical chest pain adequately and in a manner that minimizes the requirement for significant opioid administration is important.
The transversus thoracic plane block (TTPB), formerly known as the parasternal plane block, is a newer regional anesthesia technique that provides analgesia to the medial anterior chest wall and may consequently decrease pulmonary morbidity and the need for large-dose opioids. Its indications include:[1]
- Sternotomy
- Sternal fractures
- Medial rib fractures
- Medial coverage for breast surgery
- Medial coverage for placement of tunneled pacemaker or implantable cardioverter-defibrillator
Sonoanatomy
Muscles
A high-frequency linear probe is best used to scan in a parasagittal fashion medial to the mid-clavicular line over ribs 3 and 4. In this approach, the pectoralis major muscle can be appreciated beneath subcutaneous tissue and overlying the ribs. The intercostal muscles lie between the ribs and superficial to the transversus thoracic muscle (TTM), a hypoechoic band that overlies the pleura (Figure 1). The transversus thoracic plane (TTP) can be found between the internal intercostal muscle and the TTM (Figure 1) and is the target for the TTPB.
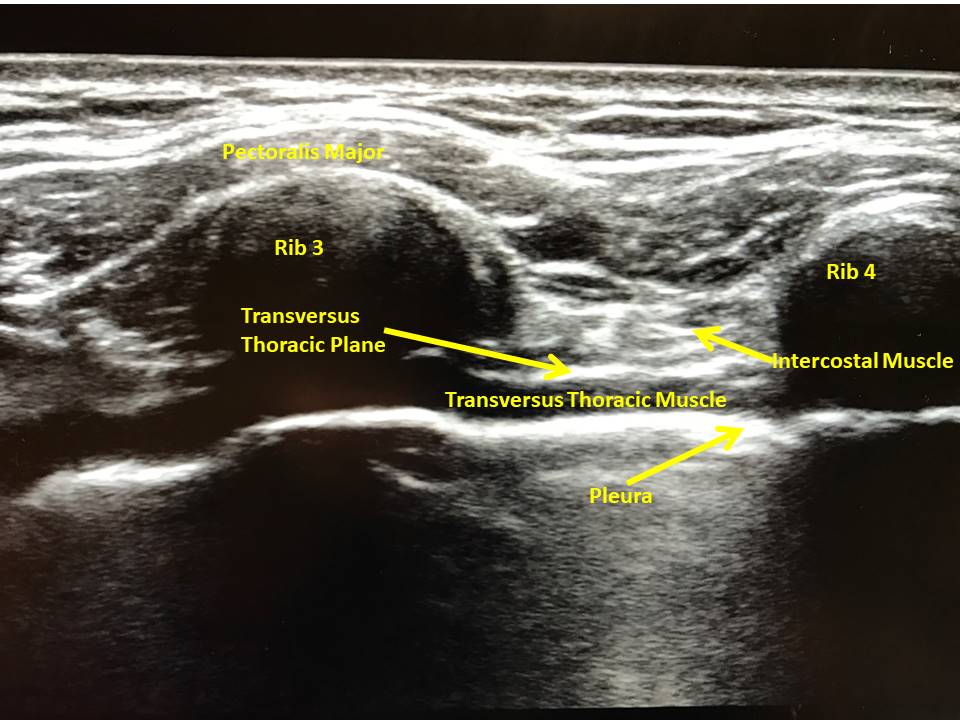 Figure 1: Ultrasound image of transversus thoracic plane with ultrasound held in longitudinal fashion over medial anterior chest wall.
Figure 1: Ultrasound image of transversus thoracic plane with ultrasound held in longitudinal fashion over medial anterior chest wall.Organs
While scanning the chest wall, the pleura is evident bilaterally as hyperechoic lines with clear lung sliding between the ribs and deep to the intercostal muscle. The pleura should move in coordination with respiratory efforts or ventricular contraction, and a lack of movement should illicit concern for pneumothorax or other pulmonary pathology. During ultrasound of the left anterior chest wall, the pericardium appears deep to the intercostal muscles. Because of these critical organs’ proximity, care must be taken to visualize the needle tip at all times. If the block cannot be performed safely, use an alternative technique.
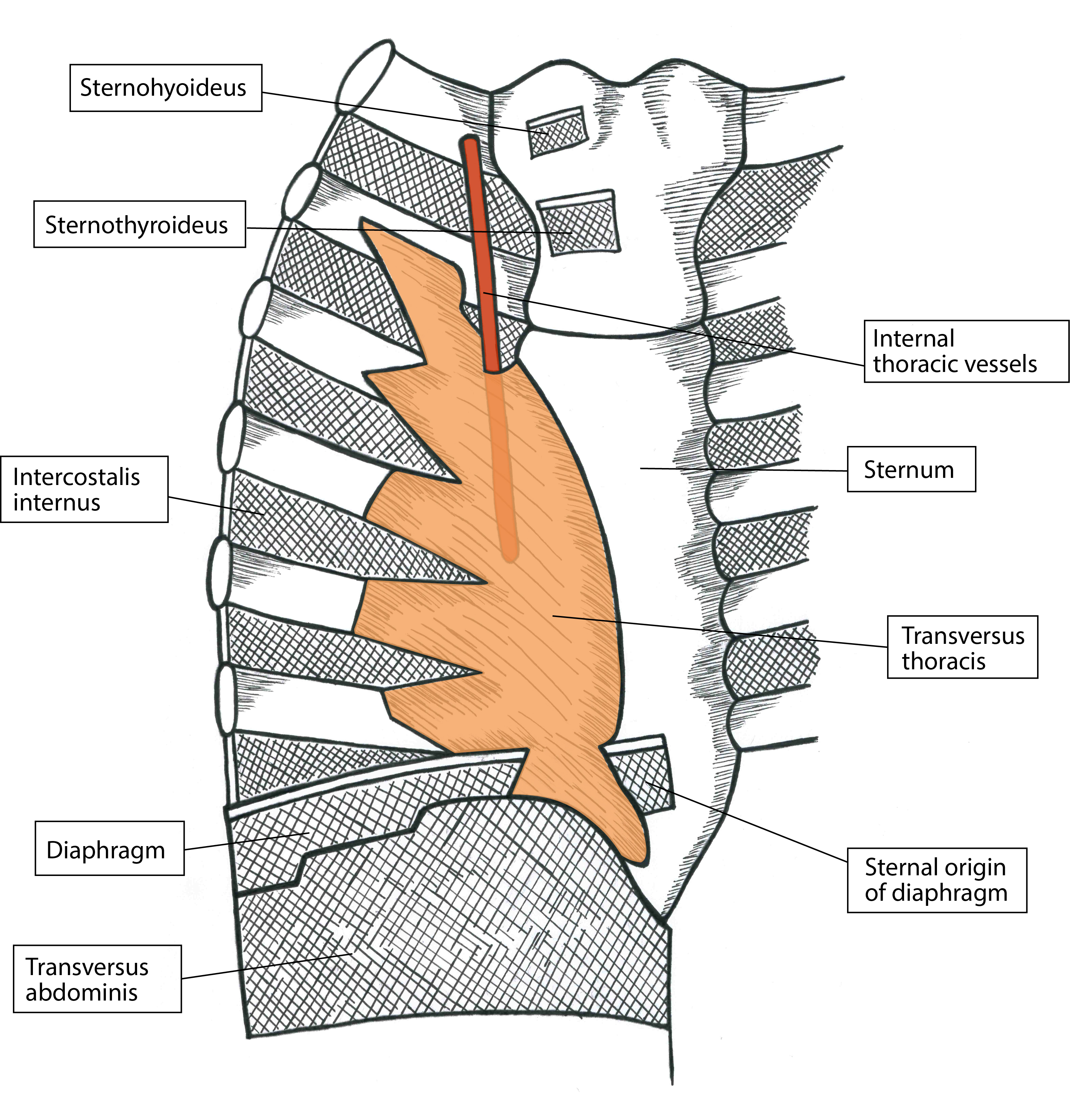
Figure 2: Artistic rendering of anterior chest wall depicting the relationship between the internal thoracic artery and transversus thoracic muscle. Artwork by Athena Ermidis.
Vessels
The internal thoracic artery runs between the internal intercostal muscles and TTM (Figure 2), and should be visualized prior to block placement. In addition to identifying the artery via longitudinal orientation of the ultrasound, placing the ultrasound in the transverse orientation over the plane of interest offers further confirmation of the arterial presence with the goal of avoidance of this vasculature.[2] Again, constant visualization of the needle tip is vital (Figure 3). Once the TTP has been accessed, aspirate every 3 to 5 mL to ensure that intravascular placement of the needle tip has not occurred. Although ASRA has neuraxial guidelines for deep plexus and deep peripheral nerve blocks, it has no defined rules for more superficial nerve blocks. However, the guidelines do advise that vascularity, compressibility, and bleeding consequences be taken into consideration.[3] We therefore recommend evaluating ease of block placement, type of anticoagulation, and vascularity of the site prior to proceeding.
Nerves
The sternum’s body derives its innervation from the anterior cutaneous branches of intercostal nerves 2–6 and the sympathetic plexus around the internal thoracic artery. The nerves lie between the internal intercostal muscle and the TTM within the TTP (Figure 4). In addition, a collateral branch also aids in supply and runs along the upper border of the rib.[4] The TTPB anesthetizes the nerves via injection of local anesthetic between the two aforementioned muscles (Figure 3). One injection into this plane on each side of the sternum between ribs 3 and 4 will spread to cover the entire sternum; multiple injections on one side of the sternum are unnecessary if the correct plane is used. Performing the block preoperatively under ultrasound guidance and appreciating no hemodynamic derangements during median sternotomy intraoperatively confirms appropriate block placement.

Figure 3: Ultrasound-guided transversus thoracic plane block.
Osseous Structures
Ideally, ribs 3 and 4 are targeted and should be visible on the ultrasound screen with an accompanying posterior acoustic shadow. Simultaneously visualize the entirety of the needle and direct it at a steep enough angle to avoid being directed beneath a rib where visualization would be obscured (Figure 3). Excessive needle insertion may result in pleural puncture or pneumothorax bilaterally, or pericardial injury on the left side of the chest.
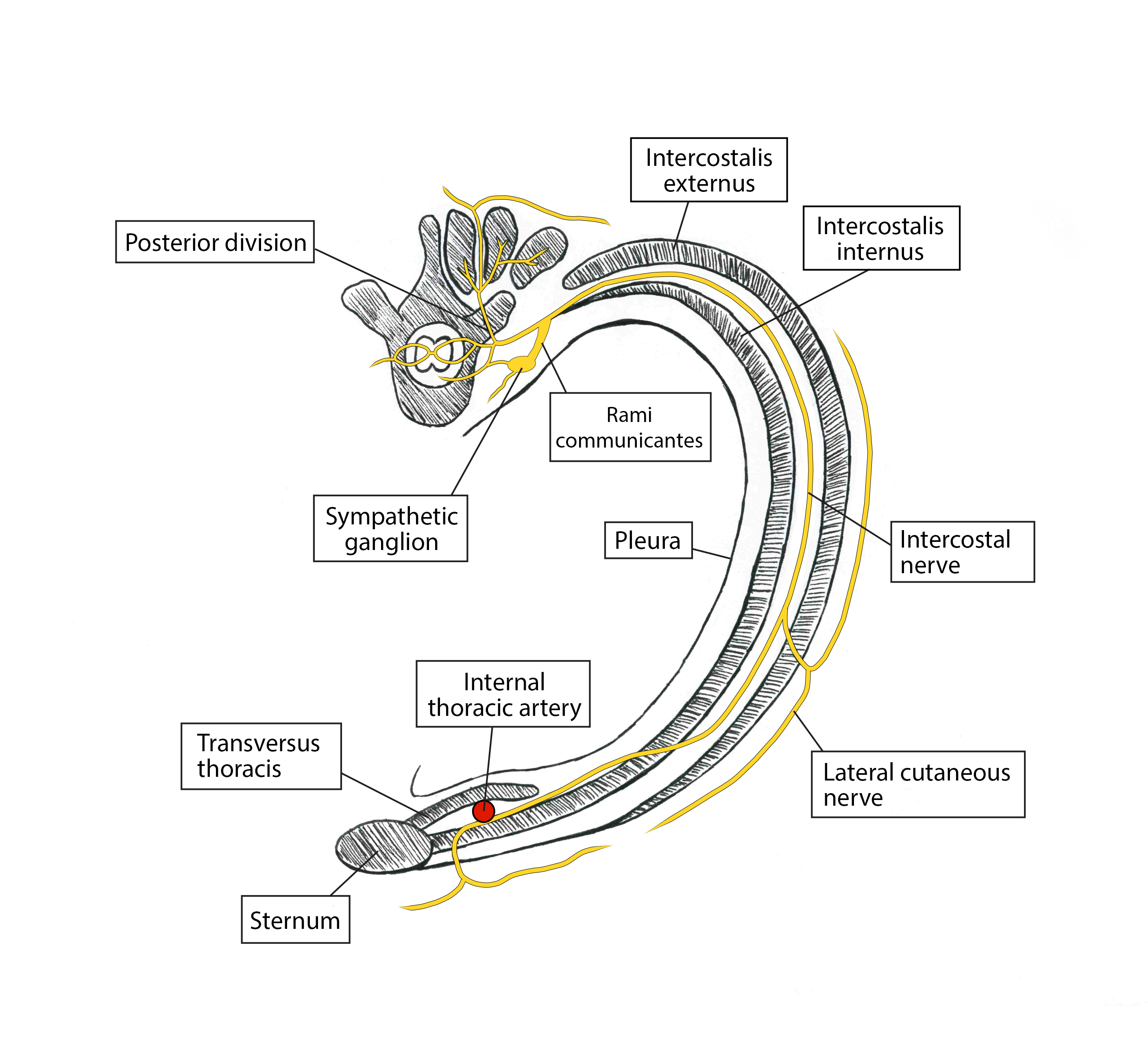
Figure 4: Artistic rendering of transverse view depicting nerve supply of anterior chest wall. Artwork by Athena Ermidis.
Patient Positioning and Equipment Selection
Needle
Use a 21-gauge, 5- or 10-cm blunt tip echogenic needle. Determine the needle length by clinical judgement based on patients’ body habitus and relevant anatomy.
Scanning Technique
Patients can be positioned either supine or with their head up to aid with respiratory status if needed. Place a 50-mm, high-frequency linear ultrasound probe on the chest in the parasagittal plane in the midclavicular line and identify the third or fourth rib space, ribs, pleura, pectoralis major, and intercostal muscles (Figure 1). Scan in a lateral to medial fashion to visualize the hypoechoic TTM lying deep to the intercostal muscle and superficial to the pleura. The needle target will be the plane between the internal intercostal muscle and the TTM (Figure 3). Care must be taken because the internal thoracic artery also runs in this plane and can be identified in cross section via an ultrasound scan in the transverse plane.[1] If a pulsatile structure is seen, place color flow doppler over the structure to confirm the presence of the artery; if the presence of vascular structures is uncertain, probe placement over an adjacent rib space to evaluate for arterial presence is recommended.
Medication Selection
Local Anesthetic
Use bupivacaine 0.25% or ropivacaine 0.25% (10–20 mL on each side). A patient’s weight, type of surgery, location of artery, and risk of vascular puncture should be considered when determining both volume and concentration of local anesthetic.
Adjuvants
Preservative-free dexamethasone (1–3 mg on each side) has anti-inflammatory properties and limits ectopic discharge in neural membranes.
Clonidine (0.5 mcg/kg with a maximum dose of 150 mcg) allows for prolongation of block via vasoconstriction secondary to hyperpolarization of gated channels. However, it has conflicting data on block duration and carries a risk of hypotension with higher doses or intravascular injection.
Epinephrine (5–10 mcg/ml) can prolong block duration via vasoconstrictive activity when used with lidocaine and mepivacaine but not ropivacaine. It has neurotoxic potential because of vasoconstriction, and hypertension and tachycardia could alert the regional team to vascular injection.
Buprenorphine can block voltage-gated sodium channels. It has antihyperalgesic properties and can prolong blocks but carries a risk of postoperative nausea and vomiting.
Limited data exist for liposomal bupivacaine, but it has not proved to be more effective or longer lasting than bupivacaine with preservative-free dexamethasone.
Nerve block catheters should be placed postoperatively to avoid surgical field contamination. Adjuvants are not required for block prolongation, but catheter migration and increased risk of infection are concerns.[5]
Description of Technique
The goal is to achieve blockade of the anterior cutaneous branches of intercostal nerves 2–6, which innervate the sternum as originally described by Ueshiema and Otake.[6] The chest is disinfected and sterile ultrasound gel is applied. A 50-mm, high-frequency linear ultrasound probe is placed on the chest in a parasagittal plane over the third and fourth ribs at the midclavicular line. The pectoralis major intercostal muscles, ribs, and pleura are identified and traced medially toward the sternum until the TTM comes into view lateral to the sternum and deep to the internal intercostal muscle as a hypoechoic band (Figure 1).
The internal thoracic artery is identified in this plane between the intercostal muscle and TTM to avoid vascular puncture and intra-arterial injection. To ensure constant visualization of the needle and prevent pericardial puncture, a blunt-tip, 21-gauge, 5- or 10-cm echogenic needle is advanced in an in-plane approach from caudal to cranial direction. The needle tip is placed between the TTM and the intercostal muscle (Figure 3). After negative aspiration, correct placement in the TTP is confirmed with 1–3 mL of sterile saline via hydrodissection followed by injection of 10–20 mL of 0.25% bupivacaine hydrochloride, or ropivacaine 0.25% with 1–3 mg of preservative-free dexamethasone in 5 mL aliquots. Downward displacement of the pleura during injection further confirms correct deposition of local anesthetic.
The maximum dose of bupivacaine hydrochloride and ropivacaine is 2.5 mg/kg of ideal body weight. In addition to the local anesthetic’s analgesic component, hydrodissection of the TTP may allow for relief of entrapment of the terminal branches of the intercostal nerves, further alleviating pain.[7]
Approach
In our practice, we approach the plane of interest in a caudal to cranial fashion. Because the rib spaces can be small in this area of the chest, moving the ultrasound transducer cranially in the parasagittal plane can help to identify the target by moving the inferior rib off of the screen. This ensures that the needle inserted in an in-plane approach is steep enough to enable the needle tip to reach the plane without bending or being inadvertently placed beneath the superior rib, where the needle tip cannot be visualized on ultrasound because of an acoustic shadow (Figure 3).
If rib spaces are narrow, limiting the angle of the needle and appropriate visualization, an out-of-plane approach may be warranted. The high-frequency linear ultrasound probe is placed in the same parasagittal orientation between ribs 3 and 4, and the TTP is identified. Using a blunt-tip 21-gauge needle, approach the TTP in an out-of-plane fashion, using sterile saline for hydrodissection to further appreciate the tip of the needle. Given that the entirety of the needle cannot be appreciated via this approach and that the tip, even using hydrodissection, can be difficult to visualize, we do not recommend this technique because of the increased risk of pneumothorax, vascular puncture, and hematoma.
Dose and Volume of Local Anesthetic
We have performed this block successfully with 10–20 mL of 0.25% bupivacaine or 0.25% ropivacaine. If the patient is having no other blocks and no intravenous local anesthetic administered, using a volume closer to 20 mL is preferable because it is a volume-dependent block. However, if the patient is of low body weight (less than 40 kilograms) or if other local anesthetics contribute to the total dose, 10 mL has provided effective analgesia in the past, anecdotally.
Block location and intercostal vasculature absorption influence its duration. It has the potential for biphasic absorption, with the initial phase occurring within 5 minutes because of the proximity of intercostal vasculature and the second slower phase resulting from the surrounding subcutaneous fat absorbing the highly lipid soluble local anesthetic.[8]
See Figure 5 for clinical pearls regarding the TTBP.

Potential Complications
Adverse events to consider include the following:
- Pneumothorax
- Hemothorax
- Pericardial puncture, resulting in potential hemopericardium or pericardial injection
- Intravascular injection
- Local anesthetic systemic toxicity
- Damage to the internal thoracic artery
- Hematoma
- Infection
- Neural injury
Conclusion
As reliance on opioids as the sole analgesic option wanes, new regional anesthesia techniques that focus on injection of local anesthetics into various fascial planes have gained prominence as critical components of multimodal analgesic regimens. Patients experiencing medial chest wall pain had not previously benefited from regional anesthesia techniques and have largely depended on intravenous and oral opioids for pain control. Although techniques that block spinal nerves (paravertebral block), or proximal intercostal nerves (intercostal block) may also be effective at treating parasternal pain, they are limited by either the potential for sympathectomy with resulting hemodynamic changes or the need to perform multiple injections to properly anesthetize a large area.
Opioid consumption has known side effects, including nausea, vomiting, decreased bowel function, diminished ventilatory drive with hypercarbia, somnolence, and tolerance and can potentially lead to problems with physical dependence or addiction. Non-opioid multimodal analgesic regimens may result in incomplete analgesia and may not be tolerated in various patient groups secondary to intolerability or side-effect profile. Epidural and paravertebral blockade require strict timing of venous thromboembolism prophylaxis protocols and may be associated with spinal hematoma and neuraxial injuries. In the authors’ experience, TTPB requires no alteration of the anticoagulant regimen, although vascularity and block difficulty should be taken into account when making a decision.
Poorly managed acute pain may ultimately result in the development of chronic pain and the need for costly and stressful additional medical or surgical intervention. “The reported incidence of chronic pain after cardiac surgery varies from 21% to 56% and is multifactorial in nature with a large neuropathic component.”[9] Therefore, the cardiac surgery population may be particularly vulnerable and warrant additional perioperative analgesic efforts.
Regional anesthesia techniques contribute to analgesia, limit the reliance on opioid medications, treat neuropathic pain, and can prevent the development of chronic pain. With such a high incidence of chronic pain in the surgical population, TTPB proves to be a useful tool in the anesthesiologist’s arsenal.
References
- Miller M, Garg J, Salter B, et al. Feasibility of subcutaneous implantable cardioverter-defibrillator implantation with opioid sparing truncal plane blocks and deep sedation. J Cardiovasc Electrophysiol. 2018;30:141–148. https://doi.org/10.1111/jce.13750
- Murata H, Hida K, Hara T. Transverse thoracic muscle plane block. Reg Anesth Pain Med. 2016;41:411–412. https://doi.org/10.1097/aap.0000000000000374
- Mittnacht A, Shariat A, Weiner M, et al. Regional techniques for cardiac and cardiac-related procedures. J Cardiothorac Vasc Anesth. 2019;33:532–546. https://doi.org/10.1053/j.jvca.2018.09.017
- Thomas K, Sainudeen S, Jose S, Nadhari M, Macaire P. Ultrasound-guided parasternal block allows optimal pain relief and ventilation improvement after a sternal fracture. Pain Ther. 2016;5:115–122. https://doi.org/10.1007/s40122-016-0050-5
- Kirksey MA, Haskins SC, Cheng J, Liu SS. Local anesthetic peripheral nerve block adjuvants for prolongation of analgesia: a systematic qualitative review. PLoS One. 2015;10:e0137312. https://doi.org/10.1371/journal.pone.0137312
- Ueshima H, Otake H. Addition of transversus thoracic muscle plane block to pectoral nerves block provides more effective perioperative pain relief than pectoral nerves block alone for breast cancer surgery. Br J Anaesth. 2017;118:439–443. https://doi.org/10.1093/bja/aew449
- Piraccini E, Biondi G, Byrne H, et al. Ultrasound guided transversus thoracic plane block, parasternal block and fascial planes hydrodissection for internal mammary post thoracotomy pain syndrome. Eur J Pain. 2018;22:1673–1677. https://doi.org/10.1002/ejp.1249
- McDonald S, Jacobsohn E, Kopacz D, et al. Parasternal block and local anesthetic infiltration with levobupivacaine after cardiac surgery with desflurane: the effect on postoperative pain, pulmonary function, and tracheal extubation times. Anesth Analg. 2005;100:25–32. https://doi.org/10.1213/01.ane.0000139652.84897.BD
- Dogan Baki E, Kavrut Ozturk N, Ayoglu R, Emmiler M, Karsli B, Uzel H. Effects of parasternal block on acute and chronic pain in patients undergoing coronary artery surgery. Semin Cardiothorac Vasc Anesth. 2016;20(3):205-212. https://doi.org/10.1177/1089253215576756
Most popular articles
How I Do It: Transversus Thoracic Plane Block
The opioid crisis currently threatening the health of the global population has compelled health care providers to reconsider appropriate analgesic options. Massive efforts have been made to maximize multimodal analgesia and regional anesthetic techniques in an attempt to reduce pain and the need for opioid analgesics. These efforts have been associated with improvements in ultrasound imaging technology and a renewed interest in anatomical study that has resulted in a proliferation of fascial plane blocks to assist in the provision of perioperative analgesia.
Although the notion of pain as the fifth vital sign now appears misguided, postsurgical pain continues to limit recovery and may increase the risk of perioperative morbidity. Poorly managed chest wall pain can contribute to an increased incidence of pulmonary complications through increased splinting. Restricted postoperative breathing can result in hypoventilation, atelectasis, pneumonia, and an increased length of hospital stay. Thus, treating surgical chest pain adequately and in a manner that minimizes the requirement for significant opioid administration is important.
Midline chest wall pain can be iatrogenic from median sternotomy and pacemaker placement, or pathologic from sternal and medial rib fractures. Chronic pain can develop following poor management of acute pain, contributing to additional physiologic and psychologic stress and consuming disproportionate physical and financial resources.
Treating surgical chest pain adequately and in a manner that minimizes the requirement for significant opioid administration is important.
The transversus thoracic plane block (TTPB), formerly known as the parasternal plane block, is a newer regional anesthesia technique that provides analgesia to the medial anterior chest wall and may consequently decrease pulmonary morbidity and the need for large-dose opioids. Its indications include:[1]
- Sternotomy
- Sternal fractures
- Medial rib fractures
- Medial coverage for breast surgery
- Medial coverage for placement of tunneled pacemaker or implantable cardioverter-defibrillator
Sonoanatomy
Muscles
A high-frequency linear probe is best used to scan in a parasagittal fashion medial to the mid-clavicular line over ribs 3 and 4. In this approach, the pectoralis major muscle can be appreciated beneath subcutaneous tissue and overlying the ribs. The intercostal muscles lie between the ribs and superficial to the transversus thoracic muscle (TTM), a hypoechoic band that overlies the pleura (Figure 1). The transversus thoracic plane (TTP) can be found between the internal intercostal muscle and the TTM (Figure 1) and is the target for the TTPB.
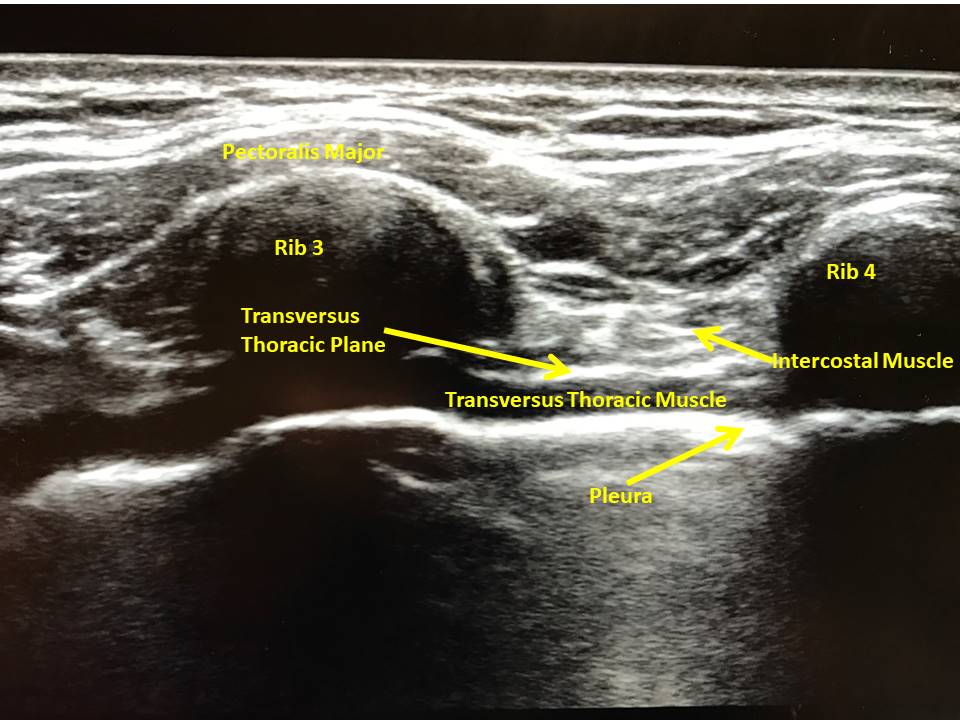 Figure 1: Ultrasound image of transversus thoracic plane with ultrasound held in longitudinal fashion over medial anterior chest wall.
Figure 1: Ultrasound image of transversus thoracic plane with ultrasound held in longitudinal fashion over medial anterior chest wall.Organs
While scanning the chest wall, the pleura is evident bilaterally as hyperechoic lines with clear lung sliding between the ribs and deep to the intercostal muscle. The pleura should move in coordination with respiratory efforts or ventricular contraction, and a lack of movement should illicit concern for pneumothorax or other pulmonary pathology. During ultrasound of the left anterior chest wall, the pericardium appears deep to the intercostal muscles. Because of these critical organs’ proximity, care must be taken to visualize the needle tip at all times. If the block cannot be performed safely, use an alternative technique.
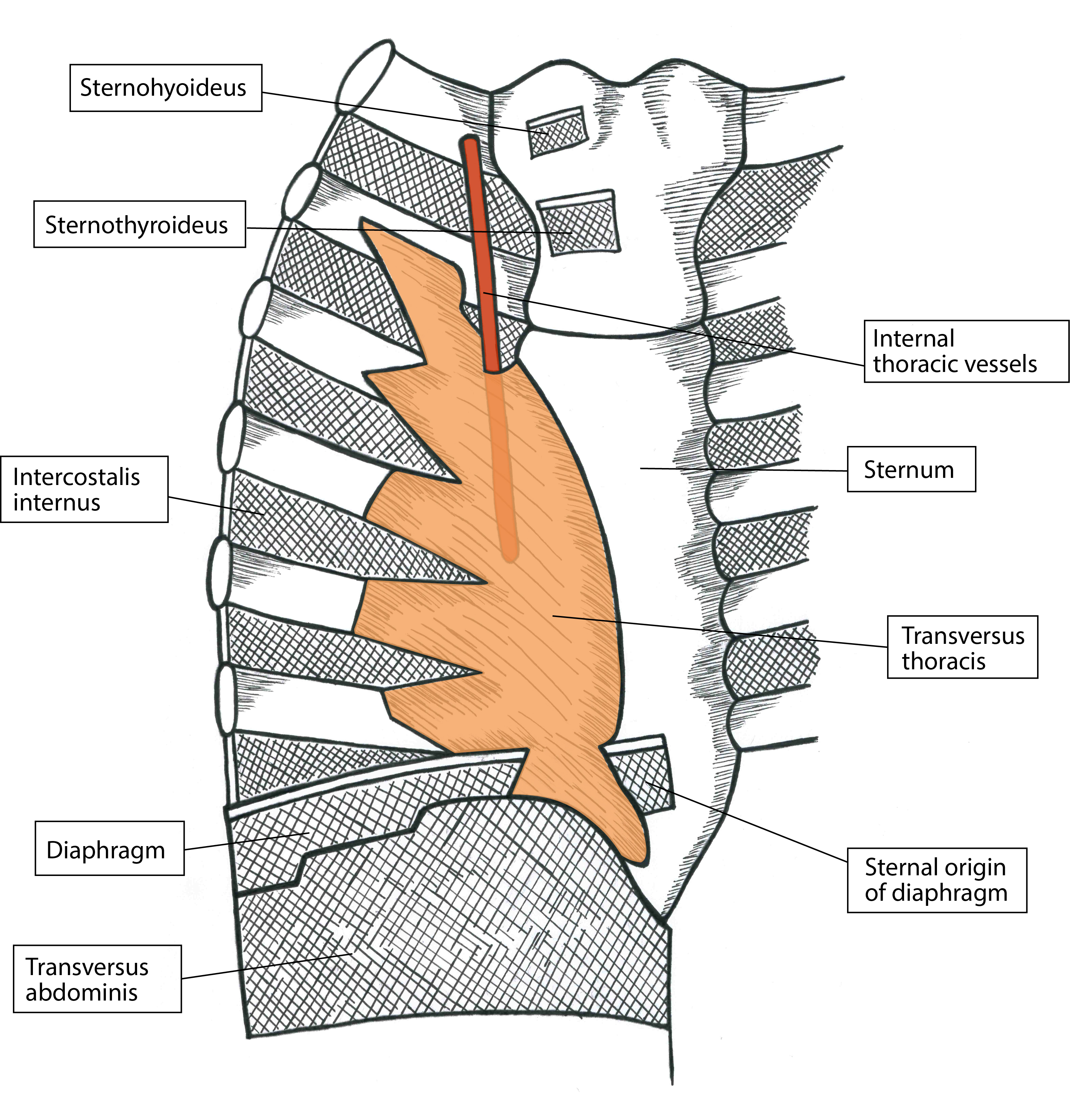
Figure 2: Artistic rendering of anterior chest wall depicting the relationship between the internal thoracic artery and transversus thoracic muscle. Artwork by Athena Ermidis.
Vessels
The internal thoracic artery runs between the internal intercostal muscles and TTM (Figure 2), and should be visualized prior to block placement. In addition to identifying the artery via longitudinal orientation of the ultrasound, placing the ultrasound in the transverse orientation over the plane of interest offers further confirmation of the arterial presence with the goal of avoidance of this vasculature.[2] Again, constant visualization of the needle tip is vital (Figure 3). Once the TTP has been accessed, aspirate every 3 to 5 mL to ensure that intravascular placement of the needle tip has not occurred. Although ASRA has neuraxial guidelines for deep plexus and deep peripheral nerve blocks, it has no defined rules for more superficial nerve blocks. However, the guidelines do advise that vascularity, compressibility, and bleeding consequences be taken into consideration.[3] We therefore recommend evaluating ease of block placement, type of anticoagulation, and vascularity of the site prior to proceeding.
Nerves
The sternum’s body derives its innervation from the anterior cutaneous branches of intercostal nerves 2–6 and the sympathetic plexus around the internal thoracic artery. The nerves lie between the internal intercostal muscle and the TTM within the TTP (Figure 4). In addition, a collateral branch also aids in supply and runs along the upper border of the rib.[4] The TTPB anesthetizes the nerves via injection of local anesthetic between the two aforementioned muscles (Figure 3). One injection into this plane on each side of the sternum between ribs 3 and 4 will spread to cover the entire sternum; multiple injections on one side of the sternum are unnecessary if the correct plane is used. Performing the block preoperatively under ultrasound guidance and appreciating no hemodynamic derangements during median sternotomy intraoperatively confirms appropriate block placement.

Figure 3: Ultrasound-guided transversus thoracic plane block.
Osseous Structures
Ideally, ribs 3 and 4 are targeted and should be visible on the ultrasound screen with an accompanying posterior acoustic shadow. Simultaneously visualize the entirety of the needle and direct it at a steep enough angle to avoid being directed beneath a rib where visualization would be obscured (Figure 3). Excessive needle insertion may result in pleural puncture or pneumothorax bilaterally, or pericardial injury on the left side of the chest.
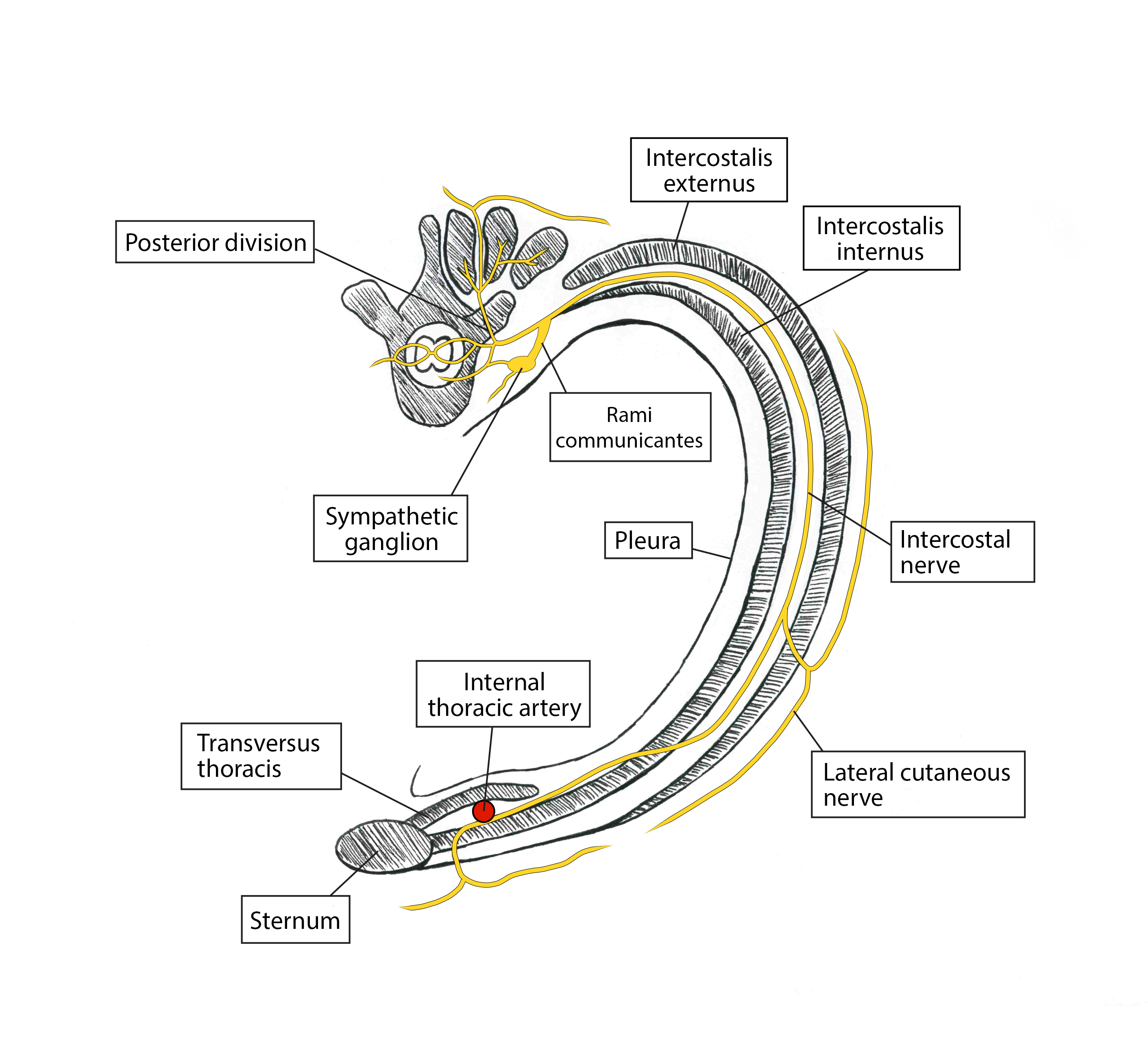
Figure 4: Artistic rendering of transverse view depicting nerve supply of anterior chest wall. Artwork by Athena Ermidis.
Patient Positioning and Equipment Selection
Needle
Use a 21-gauge, 5- or 10-cm blunt tip echogenic needle. Determine the needle length by clinical judgement based on patients’ body habitus and relevant anatomy.
Scanning Technique
Patients can be positioned either supine or with their head up to aid with respiratory status if needed. Place a 50-mm, high-frequency linear ultrasound probe on the chest in the parasagittal plane in the midclavicular line and identify the third or fourth rib space, ribs, pleura, pectoralis major, and intercostal muscles (Figure 1). Scan in a lateral to medial fashion to visualize the hypoechoic TTM lying deep to the intercostal muscle and superficial to the pleura. The needle target will be the plane between the internal intercostal muscle and the TTM (Figure 3). Care must be taken because the internal thoracic artery also runs in this plane and can be identified in cross section via an ultrasound scan in the transverse plane.[1] If a pulsatile structure is seen, place color flow doppler over the structure to confirm the presence of the artery; if the presence of vascular structures is uncertain, probe placement over an adjacent rib space to evaluate for arterial presence is recommended.
Medication Selection
Local Anesthetic
Use bupivacaine 0.25% or ropivacaine 0.25% (10–20 mL on each side). A patient’s weight, type of surgery, location of artery, and risk of vascular puncture should be considered when determining both volume and concentration of local anesthetic.
Adjuvants
Preservative-free dexamethasone (1–3 mg on each side) has anti-inflammatory properties and limits ectopic discharge in neural membranes.
Clonidine (0.5 mcg/kg with a maximum dose of 150 mcg) allows for prolongation of block via vasoconstriction secondary to hyperpolarization of gated channels. However, it has conflicting data on block duration and carries a risk of hypotension with higher doses or intravascular injection.
Epinephrine (5–10 mcg/ml) can prolong block duration via vasoconstrictive activity when used with lidocaine and mepivacaine but not ropivacaine. It has neurotoxic potential because of vasoconstriction, and hypertension and tachycardia could alert the regional team to vascular injection.
Buprenorphine can block voltage-gated sodium channels. It has antihyperalgesic properties and can prolong blocks but carries a risk of postoperative nausea and vomiting.
Limited data exist for liposomal bupivacaine, but it has not proved to be more effective or longer lasting than bupivacaine with preservative-free dexamethasone.
Nerve block catheters should be placed postoperatively to avoid surgical field contamination. Adjuvants are not required for block prolongation, but catheter migration and increased risk of infection are concerns.[5]
Description of Technique
The goal is to achieve blockade of the anterior cutaneous branches of intercostal nerves 2–6, which innervate the sternum as originally described by Ueshiema and Otake.[6] The chest is disinfected and sterile ultrasound gel is applied. A 50-mm, high-frequency linear ultrasound probe is placed on the chest in a parasagittal plane over the third and fourth ribs at the midclavicular line. The pectoralis major intercostal muscles, ribs, and pleura are identified and traced medially toward the sternum until the TTM comes into view lateral to the sternum and deep to the internal intercostal muscle as a hypoechoic band (Figure 1).
The internal thoracic artery is identified in this plane between the intercostal muscle and TTM to avoid vascular puncture and intra-arterial injection. To ensure constant visualization of the needle and prevent pericardial puncture, a blunt-tip, 21-gauge, 5- or 10-cm echogenic needle is advanced in an in-plane approach from caudal to cranial direction. The needle tip is placed between the TTM and the intercostal muscle (Figure 3). After negative aspiration, correct placement in the TTP is confirmed with 1–3 mL of sterile saline via hydrodissection followed by injection of 10–20 mL of 0.25% bupivacaine hydrochloride, or ropivacaine 0.25% with 1–3 mg of preservative-free dexamethasone in 5 mL aliquots. Downward displacement of the pleura during injection further confirms correct deposition of local anesthetic.
The maximum dose of bupivacaine hydrochloride and ropivacaine is 2.5 mg/kg of ideal body weight. In addition to the local anesthetic’s analgesic component, hydrodissection of the TTP may allow for relief of entrapment of the terminal branches of the intercostal nerves, further alleviating pain.[7]
Approach
In our practice, we approach the plane of interest in a caudal to cranial fashion. Because the rib spaces can be small in this area of the chest, moving the ultrasound transducer cranially in the parasagittal plane can help to identify the target by moving the inferior rib off of the screen. This ensures that the needle inserted in an in-plane approach is steep enough to enable the needle tip to reach the plane without bending or being inadvertently placed beneath the superior rib, where the needle tip cannot be visualized on ultrasound because of an acoustic shadow (Figure 3).
If rib spaces are narrow, limiting the angle of the needle and appropriate visualization, an out-of-plane approach may be warranted. The high-frequency linear ultrasound probe is placed in the same parasagittal orientation between ribs 3 and 4, and the TTP is identified. Using a blunt-tip 21-gauge needle, approach the TTP in an out-of-plane fashion, using sterile saline for hydrodissection to further appreciate the tip of the needle. Given that the entirety of the needle cannot be appreciated via this approach and that the tip, even using hydrodissection, can be difficult to visualize, we do not recommend this technique because of the increased risk of pneumothorax, vascular puncture, and hematoma.
Dose and Volume of Local Anesthetic
We have performed this block successfully with 10–20 mL of 0.25% bupivacaine or 0.25% ropivacaine. If the patient is having no other blocks and no intravenous local anesthetic administered, using a volume closer to 20 mL is preferable because it is a volume-dependent block. However, if the patient is of low body weight (less than 40 kilograms) or if other local anesthetics contribute to the total dose, 10 mL has provided effective analgesia in the past, anecdotally.
Block location and intercostal vasculature absorption influence its duration. It has the potential for biphasic absorption, with the initial phase occurring within 5 minutes because of the proximity of intercostal vasculature and the second slower phase resulting from the surrounding subcutaneous fat absorbing the highly lipid soluble local anesthetic.[8]
See Figure 5 for clinical pearls regarding the TTBP.

Potential Complications
Adverse events to consider include the following:
- Pneumothorax
- Hemothorax
- Pericardial puncture, resulting in potential hemopericardium or pericardial injection
- Intravascular injection
- Local anesthetic systemic toxicity
- Damage to the internal thoracic artery
- Hematoma
- Infection
- Neural injury
Conclusion
As reliance on opioids as the sole analgesic option wanes, new regional anesthesia techniques that focus on injection of local anesthetics into various fascial planes have gained prominence as critical components of multimodal analgesic regimens. Patients experiencing medial chest wall pain had not previously benefited from regional anesthesia techniques and have largely depended on intravenous and oral opioids for pain control. Although techniques that block spinal nerves (paravertebral block), or proximal intercostal nerves (intercostal block) may also be effective at treating parasternal pain, they are limited by either the potential for sympathectomy with resulting hemodynamic changes or the need to perform multiple injections to properly anesthetize a large area.
Opioid consumption has known side effects, including nausea, vomiting, decreased bowel function, diminished ventilatory drive with hypercarbia, somnolence, and tolerance and can potentially lead to problems with physical dependence or addiction. Non-opioid multimodal analgesic regimens may result in incomplete analgesia and may not be tolerated in various patient groups secondary to intolerability or side-effect profile. Epidural and paravertebral blockade require strict timing of venous thromboembolism prophylaxis protocols and may be associated with spinal hematoma and neuraxial injuries. In the authors’ experience, TTPB requires no alteration of the anticoagulant regimen, although vascularity and block difficulty should be taken into account when making a decision.
Poorly managed acute pain may ultimately result in the development of chronic pain and the need for costly and stressful additional medical or surgical intervention. “The reported incidence of chronic pain after cardiac surgery varies from 21% to 56% and is multifactorial in nature with a large neuropathic component.”[9] Therefore, the cardiac surgery population may be particularly vulnerable and warrant additional perioperative analgesic efforts.
Regional anesthesia techniques contribute to analgesia, limit the reliance on opioid medications, treat neuropathic pain, and can prevent the development of chronic pain. With such a high incidence of chronic pain in the surgical population, TTPB proves to be a useful tool in the anesthesiologist’s arsenal.
References
- Miller M, Garg J, Salter B, et al. Feasibility of subcutaneous implantable cardioverter-defibrillator implantation with opioid sparing truncal plane blocks and deep sedation. J Cardiovasc Electrophysiol. 2018;30:141–148. https://doi.org/10.1111/jce.13750
- Murata H, Hida K, Hara T. Transverse thoracic muscle plane block. Reg Anesth Pain Med. 2016;41:411–412. https://doi.org/10.1097/aap.0000000000000374
- Mittnacht A, Shariat A, Weiner M, et al. Regional techniques for cardiac and cardiac-related procedures. J Cardiothorac Vasc Anesth. 2019;33:532–546. https://doi.org/10.1053/j.jvca.2018.09.017
- Thomas K, Sainudeen S, Jose S, Nadhari M, Macaire P. Ultrasound-guided parasternal block allows optimal pain relief and ventilation improvement after a sternal fracture. Pain Ther. 2016;5:115–122. https://doi.org/10.1007/s40122-016-0050-5
- Kirksey MA, Haskins SC, Cheng J, Liu SS. Local anesthetic peripheral nerve block adjuvants for prolongation of analgesia: a systematic qualitative review. PLoS One. 2015;10:e0137312. https://doi.org/10.1371/journal.pone.0137312
- Ueshima H, Otake H. Addition of transversus thoracic muscle plane block to pectoral nerves block provides more effective perioperative pain relief than pectoral nerves block alone for breast cancer surgery. Br J Anaesth. 2017;118:439–443. https://doi.org/10.1093/bja/aew449
- Piraccini E, Biondi G, Byrne H, et al. Ultrasound guided transversus thoracic plane block, parasternal block and fascial planes hydrodissection for internal mammary post thoracotomy pain syndrome. Eur J Pain. 2018;22:1673–1677. https://doi.org/10.1002/ejp.1249
- McDonald S, Jacobsohn E, Kopacz D, et al. Parasternal block and local anesthetic infiltration with levobupivacaine after cardiac surgery with desflurane: the effect on postoperative pain, pulmonary function, and tracheal extubation times. Anesth Analg. 2005;100:25–32. https://doi.org/10.1213/01.ane.0000139652.84897.BD
- Dogan Baki E, Kavrut Ozturk N, Ayoglu R, Emmiler M, Karsli B, Uzel H. Effects of parasternal block on acute and chronic pain in patients undergoing coronary artery surgery. Semin Cardiothorac Vasc Anesth. 2016;20(3):205-212. https://doi.org/10.1177/1089253215576756

Leave a commentOrder by
Newest on top Oldest on top