View by publication date
(most recent on top)
Latest articles
How I Do It: Erector Spinae Block for Rib Fractures: The Penn State Health Experience
Introduction
Rib fractures are common in multitrauma patients and require effective analgesia to prevent respiratory complications. At the Penn State Health Milton S. Hershey Medical Center, all multitrauma patients with rib fractures are referred to the acute pain medicine service (APMS) once they have been assessed and stabilized by the trauma surgery service. APMS performs a detailed history and physical examination, focusing on location of fractures, medications, patient's current coagulation status, allergies, and other injuries, including trauma to internal abdominal organs, spine, pelvis, or limbs. APMS also evaluates history of prior surgeries or disease and mental status. An analgesic plan is formulated with the goals of optimizing respiratory function, minimizing opioid consumption, and preventing cognitive dysfunction. Therefore, the plan usually includes an interventional regional anesthesia procedure.
“The erector spinae plane (ESP) block was described in 2016 as a novel regional anesthetic technique for acute and chronic thoracic pain.”
Until recently, APMS performed mainly thoracic epidural, thoracic paravertebral, and intercostal blocks to provide rib fracture analgesia.[1-2] In general, patients with one to two rib fractures were considered for intercostal blocks, whereas patients with three or more rib fractures were considered for thoracic epidural or paravertebral blocks. However, the latter two techniques are not always feasible because of various factors, including pre-existing anticoagulation or antiplatelet therapy, hemodynamic instability, or other associated injuries (eg, vertebral fractures).

Figure 1. After patients are positioned optimally (sitting or lateral decubitus), the affected area is identified along with the target transverse process.
The erector spinae plane (ESP) block was described in 2016 as a novel regional anesthetic technique for acute and chronic thoracic pain.[3-4] It is a paraspinal fascial plane block that involves injection of local anesthetic deep in the erector spinae muscle and superficial to the tips of the thoracic transverse processes. The site of injection is distant from the pleura, major blood vessels, and spinal cord; hence, performing the ESP block has relatively few contraindications. The ESP block is less difficult to perform relative to thoracic epidural anesthesia and thoracic paravertebral block. Also, significant cranial-caudal spread occurs from a single injection point, which is an additional advantage in the setting of multiple rib fractures.
The mechanism of analgesic action is believed to result from diffusion of local anesthetic anteriorly to the ventral and dorsal rami of spinal nerves. Since its description in 2016, our practice has evolved to incorporate ESP blockade as the first-line intervention in patients with multiple rib fractures.
Single-Shot ESP Versus Continuous Catheter Block. We initially began with single-shot ESP blocks for rib fractures. However, we found that although this improved the pain and effectiveness of breathing significantly, the pain often recurred within 2 to 3 hours of the block, despite the use of long-acting local anesthetics. We postulated that systemic absorption of local anesthetic may be a contributing factor to the shorter-than-expected duration. This led to our current practice of inserting a catheter in all our patients, which has allowed us to provide prolonged analgesia.
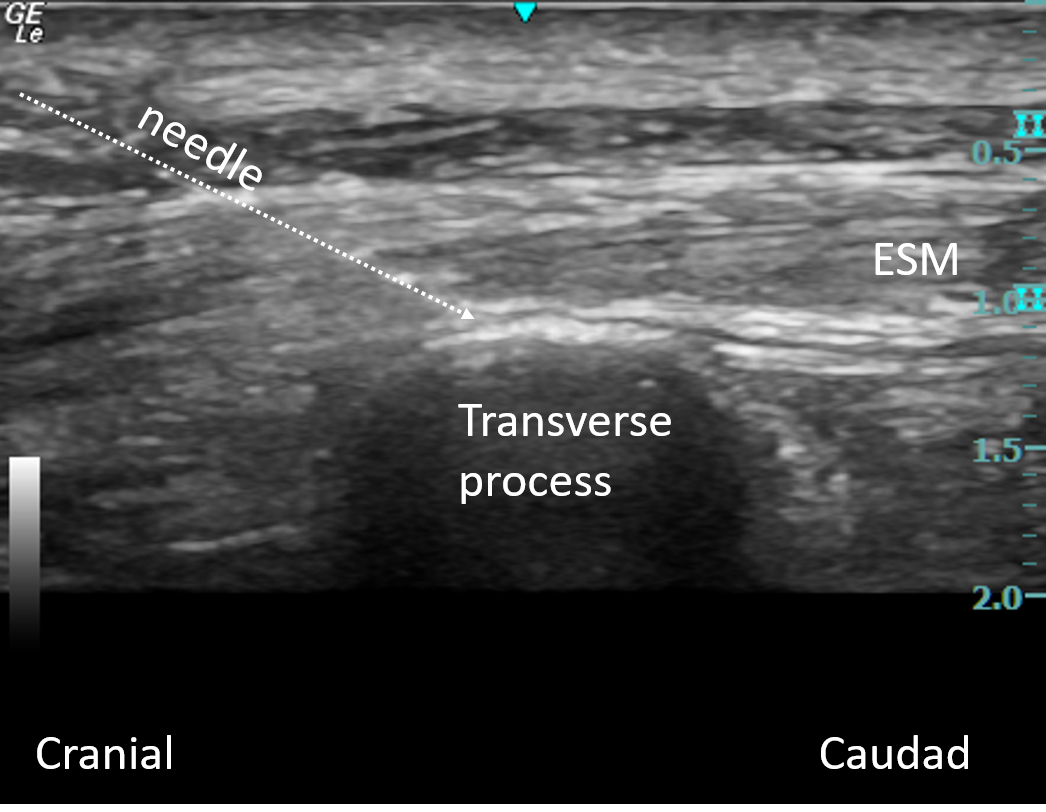
Figure 2. Transverse processes in an in-plane approach are recognizable as flat, squared-off acoustic shadows with a faint image of the pleura.
Continuous Catheter Infusion Regimens. We initially used a continuous infusion regimen of ropivacaine 0.2% at 8–10 ml/h with patient-controlled regional analgesia (PCRA) boluses of 8 ml every 60 minutes. However, we observed that patients reported significantly lower pain scores at rest and improved respiration after the bolus doses. We have therefore moved to a programmed intermittent bolus regimen of 15 ml of 0.2% ropivacaine every 3 hours with additional patient-controlled boluses of 5 ml every 60 minutes, resulting in superior analgesia and patient satisfaction.
The ESP Block Technique
Patient Selection. Any patient with three or more rib fractures, either unilateral or bilateral, is a candidate for ESP blockade. A thorough history, physical exam, and informed consent are carried out. Altered mental status, concomitant injuries, and intubation/ ventilation are considerations primarily with regard to the ability to position the patient safely and access the paraspinal area to perform the block. Unlike thoracic epidurals, the ESP block may be performed in patients with pre-existing thoracic spine disease or thoracic vertebral (ie, spinous process or lamina) fractures. Pleural puncture and pneumothorax are not significant concerns, given that the site of injection is distant from the pleura. We do not view coagulopathy or the use of anticoagulants or antiplatelet drugs as absolute contraindications to ESP block because the theoretical risk of clinically significant hemorrhage or hematoma is very low; however, an individualized risk-benefit assessment should be performed for every patient.
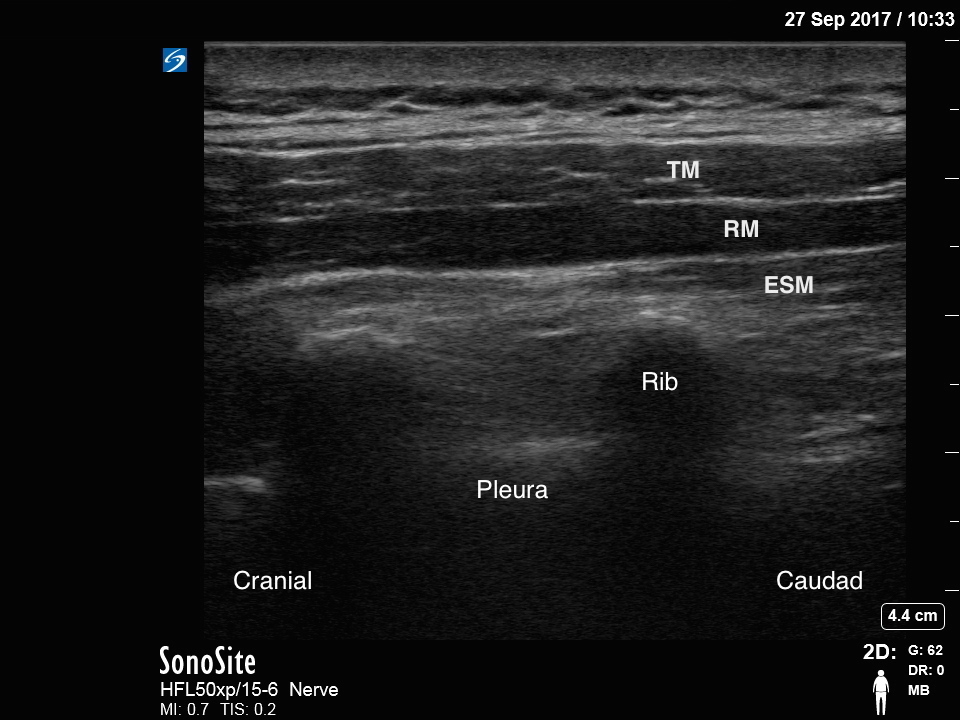
Figure 3A

Figure 3B
Figure 3. If the transducer is too lateral, the ribs will be visualized instead; these are recognizable as rounded acoustic shadows with an intervening hyperechoic pleural line (Figure 3A). If the transducer is too medial, the thoracic laminae (flat hyperechoic lines) will be visualized (Figure 3B).
Block Equipment and Preparation. In the majority of patients, we use a high-frequency (10–15 MHz) linear-array transducer because it provides a higher-resolution image; however, a low-frequency (5–2 MHz) curvilinear probe is useful in more obese patients where the transverse processes lie at a depth greater than 4 cm. We prefer to use the catheter-over-needle kit (Pajunk E-Cath, Pajunk Medical Systems, Norcross, Georgia) because they are more kink resistant. The block is performed with full aseptic precautions, and the usual precautions for any regional anesthesia procedures should be applied.
Scanning Technique. After patients are positioned optimally (sitting or lateral decubitus), the affected area is identified along with the target transverse process (Figure 1). Given that local anesthetic spreads cranially and caudally from the point of injection, this is usually the transverse process most central to the affected rib levels. The ultrasound transducer is placed in a longitudinal parasagittal orientation, about 3 cm lateral to the spinous processes, allowing for visualization of adjacent transverse processes (TP) in an in-plane approach. These are recognizable as flat, squared-off acoustic shadows with only a very faint image of the pleura visible (Figure 2). If the transducer is too lateral, the ribs will be visualized instead; these are recognizable as rounded acoustic shadows with an intervening hyperechoic pleural line (Figure 3A). If the transducer is too medial, the thoracic laminae (flat hyperechoic lines) will be visualized (Figure 3B).
After correct TP identification, an 18-gauge echogenic needle (Pajunk E-Cath, Pajunk Medical Systems) is inserted using an in-plane, cranial-to-caudad approach to contact the bony shadow of the TP with the tip deep to the fascial plane of the erector spinae muscle (Figure 4). The correct location of the needle tip is confirmed by injecting 0.5–1 cc of normal saline 0.9% and observing linear fluid spread lifting the erector spinae muscle off the tip of the TP (Figure 5). Once the fascial plane is recognized, the needle is removed and the catheter is inserted through the needle sheath. Correct catheter location is confirmed by bolusing 2–3 cc of normal saline 0.9%. Following confirmation of correct catheter tip location, 20 cc of ropivacaine 0.5% is injected and cranial and caudal spread of local anesthetic can be visualized.

Figure 4. After correct transverse process (TP) identification, an 18-gauge echogenic needle is inserted using an in-plane, cranial-to-caudad approach to contact the bony shadow of the TP with the tip deep to the fascial plane of the erector spinae muscle.

Figure 5. The correct location of the needle tip is confirmed by injecting 0.5–1 cc of normal saline 0.9% and observing linear fluid spread lifting the erector spinae muscle off the tip of the TP.
ESP Catheter Management and Follow-Up.The APMS team assesses patients daily, focusing on pain scores, incentive spirometry outcomes, ambulation status, 24-hour opioid requirements, mental status, and the integrity of the catheter insertion site. The anesthesia on-call team gets a thorough sign-out and manages any issues overnight, these may include infusion pump malfunction, inadequate analgesia, and inadvertent catheter removal. Breakthrough pain is managed with small doses of intravenous opioids. We have observed fewer instances of inadequate analgesia with the programmed intermittent bolus regimen. Using a catheter fixation device and meticulous dressing at the time of placement has reduced catheter dislodgement rates (Figures 6A and B).

6A

6B
Figure 6. Breakthrough pain is managed with small doses of IV opioid using programmed intermittent bolus. Using a catheter fixation device and meticulous dressing at the time of placement has reduced catheter dislodgement rates.
The APMS team communicates daily with the trauma surgery team regarding progress and discharge planning. The ESP catheter is kept in place as long as it is providing analgesic benefit. Factors such as respiratory status, ambulation, oral intake of medications, and chest tube removal are taken into account when deciding when to remove the ESP catheter. The catheter may also be removed if the site becomes infected, local anesthetic leaks, or at the patient's request. Currently, patients are not routinely discharged with ESP catheters in situ, although we have occasionally done so in selected patients who we judge are able to safely manage an ambulatory infusion of local anesthetic.
References
- Karmakar MK, Ho AM-H. Acute pain management of patients with multiple fractured ribs. J Trauma. 2003;54:615–625.
- Malekpour M, Hashmi A, Dove J, et al. Analgesic choice in management of rib fractures: paravertebral block or epidural analgesia? Anesth Analg. 2017;124(6):1906–1911.
- Forero M, Adhikary SD, Lopez H, et al. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41(5):621–627.
- Hamilton DL, Manickam B. Erector spinae plane block for pain relief in rib fractures. Br J Anaesth. 2017;118(3):474–475.
Most popular articles
How I Do It: Erector Spinae Block for Rib Fractures: The Penn State Health Experience
Introduction
Rib fractures are common in multitrauma patients and require effective analgesia to prevent respiratory complications. At the Penn State Health Milton S. Hershey Medical Center, all multitrauma patients with rib fractures are referred to the acute pain medicine service (APMS) once they have been assessed and stabilized by the trauma surgery service. APMS performs a detailed history and physical examination, focusing on location of fractures, medications, patient's current coagulation status, allergies, and other injuries, including trauma to internal abdominal organs, spine, pelvis, or limbs. APMS also evaluates history of prior surgeries or disease and mental status. An analgesic plan is formulated with the goals of optimizing respiratory function, minimizing opioid consumption, and preventing cognitive dysfunction. Therefore, the plan usually includes an interventional regional anesthesia procedure.
“The erector spinae plane (ESP) block was described in 2016 as a novel regional anesthetic technique for acute and chronic thoracic pain.”
Until recently, APMS performed mainly thoracic epidural, thoracic paravertebral, and intercostal blocks to provide rib fracture analgesia.[1-2] In general, patients with one to two rib fractures were considered for intercostal blocks, whereas patients with three or more rib fractures were considered for thoracic epidural or paravertebral blocks. However, the latter two techniques are not always feasible because of various factors, including pre-existing anticoagulation or antiplatelet therapy, hemodynamic instability, or other associated injuries (eg, vertebral fractures).

Figure 1. After patients are positioned optimally (sitting or lateral decubitus), the affected area is identified along with the target transverse process.
The erector spinae plane (ESP) block was described in 2016 as a novel regional anesthetic technique for acute and chronic thoracic pain.[3-4] It is a paraspinal fascial plane block that involves injection of local anesthetic deep in the erector spinae muscle and superficial to the tips of the thoracic transverse processes. The site of injection is distant from the pleura, major blood vessels, and spinal cord; hence, performing the ESP block has relatively few contraindications. The ESP block is less difficult to perform relative to thoracic epidural anesthesia and thoracic paravertebral block. Also, significant cranial-caudal spread occurs from a single injection point, which is an additional advantage in the setting of multiple rib fractures.
The mechanism of analgesic action is believed to result from diffusion of local anesthetic anteriorly to the ventral and dorsal rami of spinal nerves. Since its description in 2016, our practice has evolved to incorporate ESP blockade as the first-line intervention in patients with multiple rib fractures.
Single-Shot ESP Versus Continuous Catheter Block. We initially began with single-shot ESP blocks for rib fractures. However, we found that although this improved the pain and effectiveness of breathing significantly, the pain often recurred within 2 to 3 hours of the block, despite the use of long-acting local anesthetics. We postulated that systemic absorption of local anesthetic may be a contributing factor to the shorter-than-expected duration. This led to our current practice of inserting a catheter in all our patients, which has allowed us to provide prolonged analgesia.
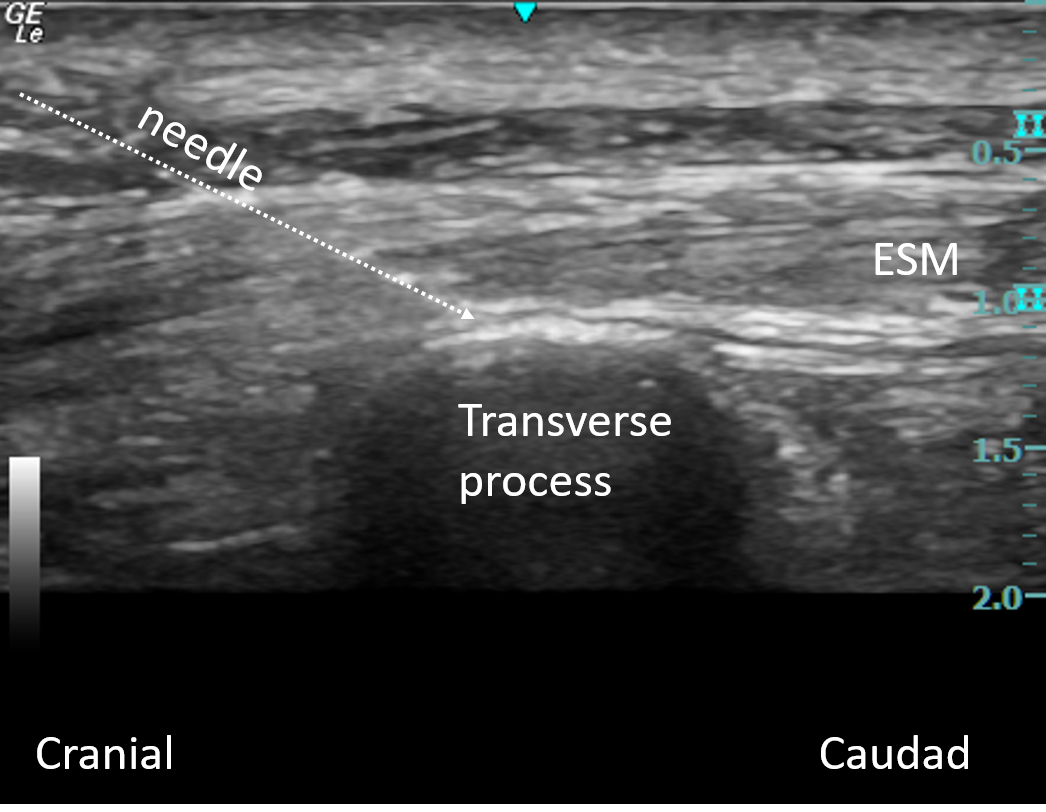
Figure 2. Transverse processes in an in-plane approach are recognizable as flat, squared-off acoustic shadows with a faint image of the pleura.
Continuous Catheter Infusion Regimens. We initially used a continuous infusion regimen of ropivacaine 0.2% at 8–10 ml/h with patient-controlled regional analgesia (PCRA) boluses of 8 ml every 60 minutes. However, we observed that patients reported significantly lower pain scores at rest and improved respiration after the bolus doses. We have therefore moved to a programmed intermittent bolus regimen of 15 ml of 0.2% ropivacaine every 3 hours with additional patient-controlled boluses of 5 ml every 60 minutes, resulting in superior analgesia and patient satisfaction.
The ESP Block Technique
Patient Selection. Any patient with three or more rib fractures, either unilateral or bilateral, is a candidate for ESP blockade. A thorough history, physical exam, and informed consent are carried out. Altered mental status, concomitant injuries, and intubation/ ventilation are considerations primarily with regard to the ability to position the patient safely and access the paraspinal area to perform the block. Unlike thoracic epidurals, the ESP block may be performed in patients with pre-existing thoracic spine disease or thoracic vertebral (ie, spinous process or lamina) fractures. Pleural puncture and pneumothorax are not significant concerns, given that the site of injection is distant from the pleura. We do not view coagulopathy or the use of anticoagulants or antiplatelet drugs as absolute contraindications to ESP block because the theoretical risk of clinically significant hemorrhage or hematoma is very low; however, an individualized risk-benefit assessment should be performed for every patient.
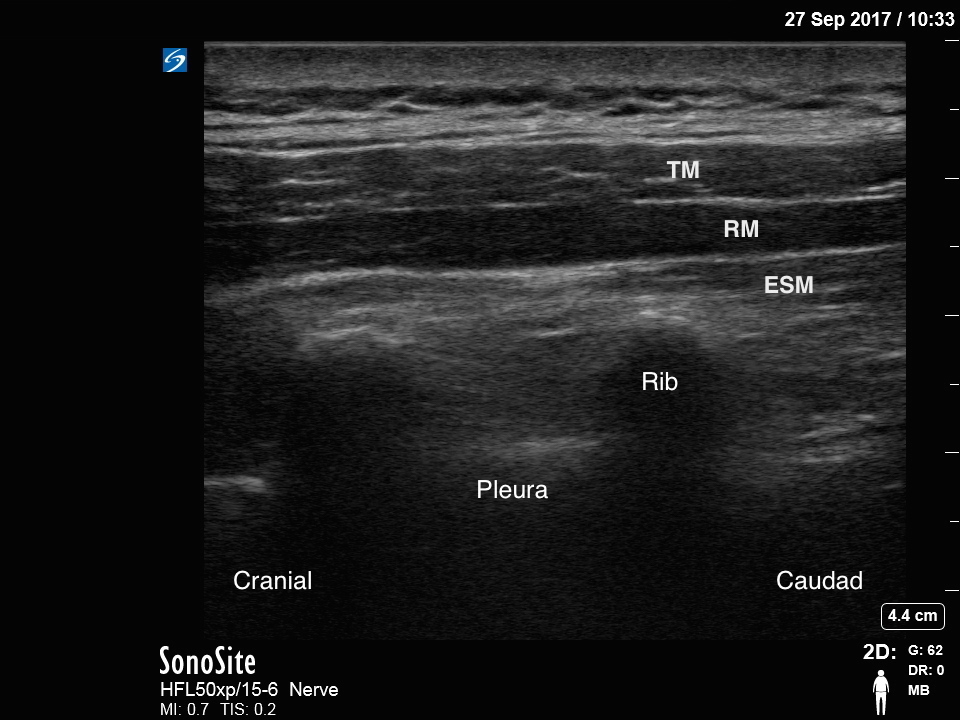
Figure 3A

Figure 3B
Figure 3. If the transducer is too lateral, the ribs will be visualized instead; these are recognizable as rounded acoustic shadows with an intervening hyperechoic pleural line (Figure 3A). If the transducer is too medial, the thoracic laminae (flat hyperechoic lines) will be visualized (Figure 3B).
Block Equipment and Preparation. In the majority of patients, we use a high-frequency (10–15 MHz) linear-array transducer because it provides a higher-resolution image; however, a low-frequency (5–2 MHz) curvilinear probe is useful in more obese patients where the transverse processes lie at a depth greater than 4 cm. We prefer to use the catheter-over-needle kit (Pajunk E-Cath, Pajunk Medical Systems, Norcross, Georgia) because they are more kink resistant. The block is performed with full aseptic precautions, and the usual precautions for any regional anesthesia procedures should be applied.
Scanning Technique. After patients are positioned optimally (sitting or lateral decubitus), the affected area is identified along with the target transverse process (Figure 1). Given that local anesthetic spreads cranially and caudally from the point of injection, this is usually the transverse process most central to the affected rib levels. The ultrasound transducer is placed in a longitudinal parasagittal orientation, about 3 cm lateral to the spinous processes, allowing for visualization of adjacent transverse processes (TP) in an in-plane approach. These are recognizable as flat, squared-off acoustic shadows with only a very faint image of the pleura visible (Figure 2). If the transducer is too lateral, the ribs will be visualized instead; these are recognizable as rounded acoustic shadows with an intervening hyperechoic pleural line (Figure 3A). If the transducer is too medial, the thoracic laminae (flat hyperechoic lines) will be visualized (Figure 3B).
After correct TP identification, an 18-gauge echogenic needle (Pajunk E-Cath, Pajunk Medical Systems) is inserted using an in-plane, cranial-to-caudad approach to contact the bony shadow of the TP with the tip deep to the fascial plane of the erector spinae muscle (Figure 4). The correct location of the needle tip is confirmed by injecting 0.5–1 cc of normal saline 0.9% and observing linear fluid spread lifting the erector spinae muscle off the tip of the TP (Figure 5). Once the fascial plane is recognized, the needle is removed and the catheter is inserted through the needle sheath. Correct catheter location is confirmed by bolusing 2–3 cc of normal saline 0.9%. Following confirmation of correct catheter tip location, 20 cc of ropivacaine 0.5% is injected and cranial and caudal spread of local anesthetic can be visualized.

Figure 4. After correct transverse process (TP) identification, an 18-gauge echogenic needle is inserted using an in-plane, cranial-to-caudad approach to contact the bony shadow of the TP with the tip deep to the fascial plane of the erector spinae muscle.

Figure 5. The correct location of the needle tip is confirmed by injecting 0.5–1 cc of normal saline 0.9% and observing linear fluid spread lifting the erector spinae muscle off the tip of the TP.
ESP Catheter Management and Follow-Up.The APMS team assesses patients daily, focusing on pain scores, incentive spirometry outcomes, ambulation status, 24-hour opioid requirements, mental status, and the integrity of the catheter insertion site. The anesthesia on-call team gets a thorough sign-out and manages any issues overnight, these may include infusion pump malfunction, inadequate analgesia, and inadvertent catheter removal. Breakthrough pain is managed with small doses of intravenous opioids. We have observed fewer instances of inadequate analgesia with the programmed intermittent bolus regimen. Using a catheter fixation device and meticulous dressing at the time of placement has reduced catheter dislodgement rates (Figures 6A and B).

6A

6B
Figure 6. Breakthrough pain is managed with small doses of IV opioid using programmed intermittent bolus. Using a catheter fixation device and meticulous dressing at the time of placement has reduced catheter dislodgement rates.
The APMS team communicates daily with the trauma surgery team regarding progress and discharge planning. The ESP catheter is kept in place as long as it is providing analgesic benefit. Factors such as respiratory status, ambulation, oral intake of medications, and chest tube removal are taken into account when deciding when to remove the ESP catheter. The catheter may also be removed if the site becomes infected, local anesthetic leaks, or at the patient's request. Currently, patients are not routinely discharged with ESP catheters in situ, although we have occasionally done so in selected patients who we judge are able to safely manage an ambulatory infusion of local anesthetic.
References
- Karmakar MK, Ho AM-H. Acute pain management of patients with multiple fractured ribs. J Trauma. 2003;54:615–625.
- Malekpour M, Hashmi A, Dove J, et al. Analgesic choice in management of rib fractures: paravertebral block or epidural analgesia? Anesth Analg. 2017;124(6):1906–1911.
- Forero M, Adhikary SD, Lopez H, et al. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41(5):621–627.
- Hamilton DL, Manickam B. Erector spinae plane block for pain relief in rib fractures. Br J Anaesth. 2017;118(3):474–475.

Leave a commentOrder by
Newest on top Oldest on top