Setting Up a Regional Anesthesia Pathway to Improve Value of Care in Upper Limb Surgery: A European Perspective
Regional anesthesia (RA) improves postoperative analgesia and can contribute to a reduction in chronic postsurgical pain, postoperative nausea and vomiting (PONV), and pulmonary complications. RA can also improve value of care by reducing length of stay, improving operating department throughput, and enhancing patient satisfaction.1 A recent perioperative observational study of 16,222 patients demonstrated that predictors of patient dissatisfaction were severe pain, drowsiness, sore throat, and PONV, all of which can potentially be eliminated using RA.2
Using RA in combination with process mapping and lean methodology in the National Health Service setting to create a streamlined perioperative pathway facilitating awake upper limb surgery improves overall value of care by improving patient experience and reducing waste, inefficiencies, and overall cost
Regional Anesthesia Service Models
Although RA block rooms are well established in North America, that model has not been widely replicated in the United Kingdom (UK). One potential contributing factor for this is the lack of a fee-for-service model in the UK; thus, there is reduced collective incentive to have a central block room feeding all operating rooms. In addition, many UK anesthesiologists prefer to perform their own nerve block procedures either in the operating room or in the adjoining anesthesia induction room. (Historically, induction rooms were used for induction of anesthesia before transferring a patient into the operating room; however, that practice is becoming less common across the UK.) Attempts to fund a North American-style block room can also meet with resistance from hospital administration.

Figure 1. The Value Equation in Healthcare From www.healthcareitnews.com/sponsored-content/solving-healthcare-value-equation-0#gs.QsPjeso. Reprinted with permission.
Implementation of a new RA service must be seen to improve value of perioperative care (See Figure 1.), therefore demonstrating quality improvement through cost reduction. Historically in our institution, RA was used by some on an ad hoc basis; however, a more structured and streamlined approach was needed. As a starting point, we reviewed the perioperative medicine and surgical home approaches to expand our intraoperative anesthetic role to the entire perioperative pathway and achieve the goals of healthcare’s triple aim.3–6 We investigated how RA could add value to the entire perioperative pathway of particular subsets of surgical procedures, from decision to operate through to the postoperative period. We saw the highest potential value gains with hand and elbow surgery and embarked on our RA service transformation by creating an awake upper limb surgery perioperative pathway.
Quality Improvement Methodology
Process mapping of our existing perioperative pathway revealed many unnecessary and inefficient steps that did not add value to the overall pathway: full preoperative assessment and investigation, full medical clerk-in on the day of surgery, induction of general anesthesia, administration of intravenous opioid analgesia, emergence from anesthesia, recovery from anesthesia, and overnight hospital stays. Using lean methodology, we eliminated the unnecessary steps and created a streamlined awake upper limb surgery pathway. (See Figure 2.)


Figure 2. Upper Limb Surgery Pathways (A) Process mapping of existing perioperative pathway for upper limb surgery; (B) lean streamlined awake upper limb surgery pathway
To further maximize value, we sought to improve operating room efficiency with concurrent use of the parallel processing model. (See Figure 3.) RA-UK guidelines state that in certain, well-defined circumstances, an anesthesiologist is not required to be present throughout surgery under peripheral nerve block.7 Therefore, for awake hand or elbow surgery, a suitably trained member of the multidisciplinary team can monitor patients while the anesthesiologist places the nerve block, thus minimizing operating room turnover time.
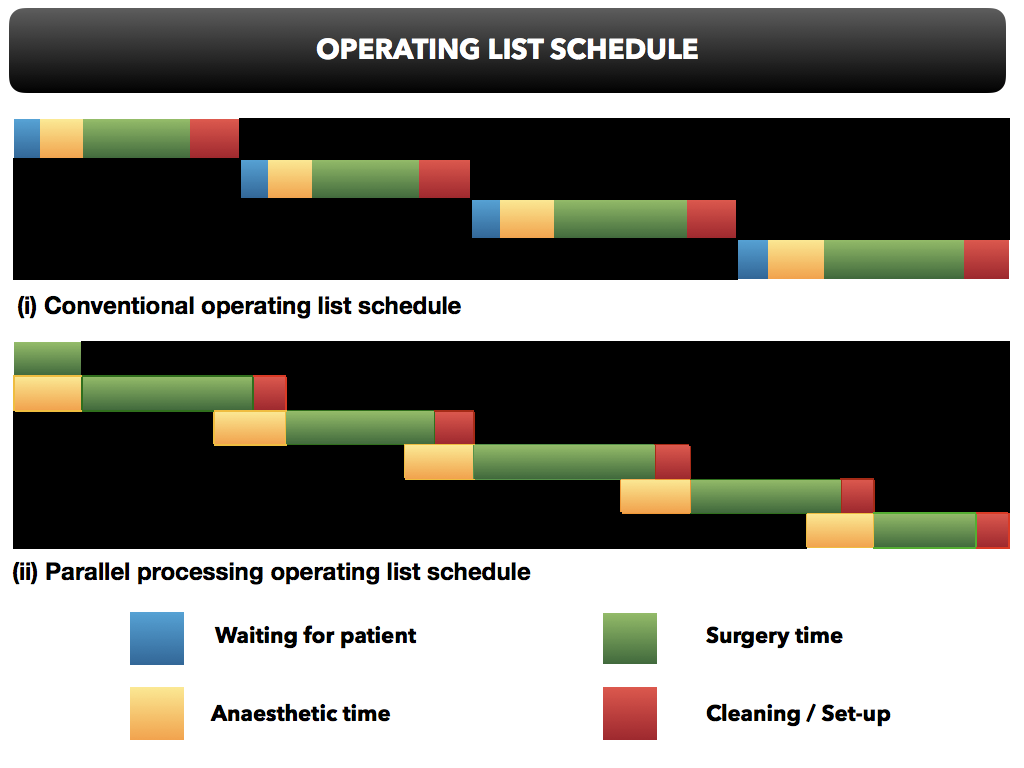
Figure 3. Parallel Processing Model Leads to Reduced Operative Turnover Time
Changing the Culture
A challenge in many institutions is developing a culture of acceptance of RA in a system where its benefits are not ubiquitously appreciated. A complete change of departmental mindset and culture is required to overcome common misconceptions that RA is unreliable, time-consuming, and contributes to delays in hospital discharge.
The surgical team needs time and a good working relationship to develop confidence that RA is effective for awake surgery and that patients are satisfied with the technique. One strategy is to target a selection of cases that are deemed too high risk for general anesthesia, allowing the surgical team to observe for itself the benefits of awake surgery. If surgical colleagues are wary of breakthrough pain following hospital discharge, patients can be admitted but only prescribed the analgesia they would receive at home. Subsequent review allows surgical team to develop confidence in the robust postoperative analgesia pathway and to hear patients expressing high levels of satisfaction with the awake surgery pathway.
Patient Expectations
Another fundamental challenge in starting an awake upper limb surgery pathway is managing patient expectations. In most units, patients arrive into hospital expecting to have general anesthesia, having been told so at the surgical booking and throughout the preoperative period. An unexpected awake surgery curveball on the morning of surgery can cause unnecessary distress and is not best practice in terms of providing informed consent, avoiding cancellations, and maintaining high levels of patient satisfaction. Patient expectations can be molded early in the perioperative pathway by providing an information pamphlet or educational video, but perhaps the most important factor is endorsement by the surgeon at the time of the surgical booking.
Preoperative Assessment
In many institutions, patients having hand or elbow surgery undergo a full comprehensive preoperative assessment including hematologic, cardiac, or respiratory investigations and sometimes even specialist referral. During the preliminary stages of our awake upper limb surgery pilot, we observed many high-risk patients who had been thoroughly investigated during the preoperative assessment and were deemed to require high dependency unit care postoperatively. Each patient subsequently underwent awake surgery under brachial plexus block and were discharged home approximately one hour postoperatively. It became clear that the traditional format of preoperative assessment was both excessive and inefficient for patients undergoing awake hand or elbow surgery.
As a result, we created a streamlined awake upper limb surgery preoperative assessment model, where no preoperative investigations are routinely ordered. During this process, we answer just three simple questions:
- Has the patient provided informed consent to have awake surgery under RA?
- Does the patient have any contraindications to having awake surgery under RA?
- Has the patient had a comprehensive medication review?
In this model, patients attend in groups, allowing 32 patents to be reviewed in a morning session. First, each group receives an explanation of the perioperative pathway for awake upper limb surgery. They are then shown a short informational video outlining each step of the pathway, followed by a group question-and-answer session. Each patient then meets individually with an anesthesiologist to review medications, including anticoagulants, and allow for any further questions on an individual basis. As a result, patients arrive on the morning of surgery with the expectation of having awake surgery.
Operating List Efficiency
Effective planning of upper limb lists is essential to maximize efficiency. In our institution, we run dedicated block lists and no routine general anesthetics are performed on those lists. To use theater time while the first nerve block is placed, a minor case such as carpal tunnel repair is performed under local anesthesia infiltration. Patient flow is crucial to successfully running the block list. This is ideally facilitated by a bespoke regional anesthesia day unit, where patients check into a large holding area near the operating suite and the nerve blocks can be performed. In some institutions, where patients are located in a ward separate from the operating complex, careful planning is required to prevent delays in transferring patients to the block room.
Peripheral Nerve Block Procedure
Prior to nerve block placement in the block room, patients are given the option to receive light sedation of up to 1 mg intravenous midazolam. Further doses may be requested, but in our experience they are very seldom required. Patients having awake surgery under brachial plexus block do not need intravenous fluids, because bladder distention can cause significant irritation. A systematic process of checking block success prior to transfer to the operating room, combined with adequate patient education, removes the need for intraoperative propofol sedation during surgery under regional anesthesia. Patients are therefore wide awake during surgery and often use a portable electronic device for entertainment. If any concerns are present following sensorimotor testing 30 minutes after block insertion, a targeted rescue block is routinely administered before transfer to the operating room, thus eliminating conversion to general anesthesia.
Postoperative Analgesia
To ensure high-quality and appropriately timed postoperative analgesia, a standardized discharge analgesia prescription with two distinct pathways (soft tissue and bony surgery) is used. The bony surgery pathway has the option of a short duration of opioid analgesia, whereas the soft tissue pathway uses simple analgesia only. Patients are instructed to take pain medications prior to resolution of the nerve block. Quality of postoperative analgesia, timing of block regression, and other patient-reported outcome measures are recorded at 48-hour follow-up telephone call.
Value of Care
To demonstrate value of care from our awake upper limb pathway, we performed a quality improvement project that does not require institutional review board approval. We evaluated three key areas:
1. Patient Experience
Patient responses on satisfaction questionnaires before and after implementation of the awake upper limb pathway demonstrated a significant reduction in pain, opioid-related side effects (eg, drowsiness, nausea, itch), and the hangover effects of anesthesia. (See Table 1.) All patients who had awake upper limb surgery stated that they would choose the technique again over general anesthesia. Reasons included the lack of hangover and drowsiness from anesthesia, the ability to eat and drink immediately, excellent pain relief, and the ability to go home within an hour of surgery.
Table 1. Patient-Reported Outcome Measures After General Anesthesia with No Nerve Block Compared to Regional Anesthesia.
Just after your surgery, how satisfied were you with……? | ||
Outcome Measure | General Anesthesia (%) | Regional Anesthesia (%) |
Pain relief | 74 | 100 |
Nausea and vomiting | 84 | 100 |
Sore throat | 76 | 100 |
Dry mouth | 66 | 96 |
Drowsiness | 70 | 100 |
Difficulty breathing | 84 | 100 |
Wearing oxygen mask | 70 | 100 |
Dizziness | 76 | 100 |
Value is defined as the percentage of patients with 5-point Likert satisfaction score of 4 and above (N = 100).
2. Efficiency
The use of parallel processing contributed to a 20-minute reduction (44 to 24 mins) in operative turnover time (time from skin closure until subsequent patient positioned and ready), which has equated to the addition of one extra case per half-day operating session. Patients now bypass the postanesthesia care unit, instead of staying an average of one hour in the previous model. Despite a more lean and simplistic form of preoperative assessment, the cancellation rate for awake surgery is now zero, compared with a previous rate of 5%–10%. Previously, all patients undergoing bony wrist surgery (eg, trapezectomy or arthrodesis wrist fusion) and approximately 45% of other hand and elbow surgery stayed at least one night in hospital. All patients are now discharged on the day of surgery unless required to stay for surgical reasons.
3. Value
Cost benefit is always an important consideration for hospital administration, especially with any new program. It is logical to assume that the increased throughput of cases and same-day hospital discharge would have cost-savings benefit. Our awake upper limb surgery pathway started with two half-day operating sessions per week. In conjunction with our trust accountant and the National Health Service tariff system, we calculated the cost savings of running a two-session block list one day per week over a one-year period. It equates to a saving of just under $400,000 per year, which is even more significant considering the concurrent improvement in patient experience. (See Table 2.)
Table 2. Estimated Cost Savings Based on Two Awake Surgery Sessions (one day) Per Week for One Year
Expense Category | Individual Cost ($) | Frequency | Cost Savings ($) |
Extra cases | 1394 | 104 | 144,976 |
Cancellations | 2219 | 21 | 46,599 |
Bed days | 799 | 125 | 99,875 |
Echocardiogram | 277 | 30 | 8310 |
Electrocardiograph | 13 | 208 | 2704 |
PACU stay | 264 | 208 | 54,912 |
Drugs and equipment | 79 | 208 | 16,432 |
Blood tests | 92 | 208 | 19,136 |
Specialist referrals | 277 | 10 | 2770 |
Information clinic | 277 | 6 | 1662 |
Total | $397,376 |
PACU, postanesthesia care unit.
Summary
Using RA in combination with process mapping and lean methodology in the National Health Service setting to create a streamlined perioperative pathway facilitating awake upper limb surgery improves overall value of care by improving patient experience and reducing waste, inefficiencies, and overall cost. (See Figure 4.) Starting a RA service transformation with a simple, lean, pathway-based approach allows a gradual positive change of culture and acceptance, on which further service development can be based.
Figure 4. Advantages of a Streamlined, Regional Anesthesia-Focused Surgical Pathway
Advantages of Awake Surgery Pathway and Block Room |
Reduces operating turnover time |
Increases operative caseload |
Allows patients to bypass postanesthesia care unit |
Eliminates day-of-surgery cancellations |
Reduces length of stay |
Avoids general anaesthesia and opioids |
Improves patient satisfaction |
Provides a teaching and research hub |
References
- Hutton, M, Brull R, McFarlane A. Regional anaesthesia and outcomes. BJA Education. 2018;18(2):52–56. https://doi.org/10.1016/j.bjae.2017.10.002
- Walker EMK, Bell M, Cook TM, Grocott MPW, Moonesinghe SR. Patient reported outcome of adult perioperative anaesthesia in the United Kingdom: a cross-sectional observational study. Br J Anaesth. 2016;117:758–766. https://doi.org/10.1093/bja/aew381
- Royal College of Anaesthetists. Perioperative medicine: the pathway to better surgical care. 2015. https://www.rcoa.ac.uk/sites/default/files/PERIOP-2014.pdf. Accessed September 9, 2018.
- Grocott MPW, Pearse RM. Perioperative medicine: the future of anaesthesia? Br J Anaesth. 2012;108(5):723–726. https://doi.org/10.1093/bja/aes124
- Vetter TR, Boudreaux AM, Jones KA, Hunter JM, Pittet JF. The perioperative surgical home: how anesthesiology can collaboratively achieve and leverage the triple aim in health care. Anesth Analg. 2014;118:1131–1136. https://doi.org/10.1213/ANE.0000000000000228
- Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff. 2008;27:759–769. https://doi.org/10.1377/hlthaff.27.3.759
- Regional Anaesthesia United Kingdom. RA-UK guidelines for supervision of patients during peripheral regional anaesthesia. 2015. https://www.ra-uk.org/index.php/guidelines-standards/5-detail/274-supervision-statement. Accessed July 3, 2018.
Leave a commentOrder by
Newest on top Oldest on top