How I Do It: Infraclavicular Block
This article originally appeared in the ASRA News,Volume 12, Issue 4, pp 17-19 (August 2012).
Author
Yavuz Gürkan, MD
Associate Professor of Anesthesiology and Reanimation
Kocaeli University Hospital
Kocaeli, Turkey
Section Editor: Steven Orebaugh, MD
Infraclavicular block (ICB) is an upper extremity block that provides complete anesthesia below the shoulder. Refinement in techniques and ultrasound (US) guidance have increased the interest in ICB, and it is probably one of the most commonly-performed upper extremity blocks today.
Anatomy
This block is performed below the clavicle at the cord level of brachial plexus. The axillary (subclavian) artery is surrounded by three cords. The axillary vein lies adjacent to the artery and is positioned caudally. These three cords - lateral, posterior and medial - are named according to their relative position to the artery. The anatomy of the plexus varies widely among individuals. The MRI study of Sauter[1] revealed that the cords are found within 2 cm from the center of the artery, approximately within 2/3 of a circle. With reference to a clock face with the axillary artery at the center, the cords are distributed between 3 and 11 o’clock. Considering all volunteers, an average point with shortest distances to all cords was found at 8 o’clock, close to the artery, in the cranioposterior quadrant.
History
ICB was first described by Bazy[2] in 1914. Although the technique has a long history, Raj[3] modified the technique and reported a high success rate using a nerve stimulator in 1973. Failure to obtain similar success rates reported by Raj has led to a search for an approach that has consistently-high success rates in different hands. Since that time, many approaches, which differ in the site of needle entry and/or needle direction, have been described.
Following MRI studies, Klaastad[4] has suggested that ICB can be accomplished by the ‘lateral sagittal route’ [lateral sagittal infraclavicular block (LSIB)] with ease and low risk of complications, such as pneumothorax or vascular puncture. LSIB is the infraclavicular approach used in our clinic. With this technique, it is easy to palpate the bony landmarks -clavicle and coracoid process- even in obese patients. Using LISB, the single injection technique is well-accepted by patients with fewer adverse effects than an axillary block by multiple-injection technique[5] and more complete anesthesia with a block onset time of 20 minutes. Large-scale studies have reported similar success rates that range between 89.5% and 91%.[6-8] This dependably-high success rate seems to be a major advantage of the LSIB technique.
Ultrasound-Guided LSIB Technique
Although LSIB was first performed using nerve stimulation (NS), it is a technique very suitable for US guidance. Important sonoanatomic structures include the axillary artery and three cords of the brachial plexus posterior to the pectoralis minor muscle.[9] Using a linear probe, the prominent pulsatile axillary artery can be easily identified. Brachial plexus cords that surround the artery look hyperechoic and can be identified with high resolution US machines. Yet, sometimes difficulty can be encountered seeing the posterior cord, which lies behind the artery and can be confused with the acoustic enhancement beyond the blood vessel (Fig. 1). Comparative studies have revealed that US guidance further increases the block success rate up to 95%.[10-11] Currently in our clinic, where more than 1000 US guided LSIB has been performed during recent years, our success rate is over 95% (unpublished data). US guidance has also reduced vascular puncture incidence from 20% to almost nil.[6,10,11] In addition to high success rates, improved patient safety, and comfort, US guidance has provided certain advantages that allow the technique to be used in many instances where it would not be clinically feasible with NS alone.[12-14]
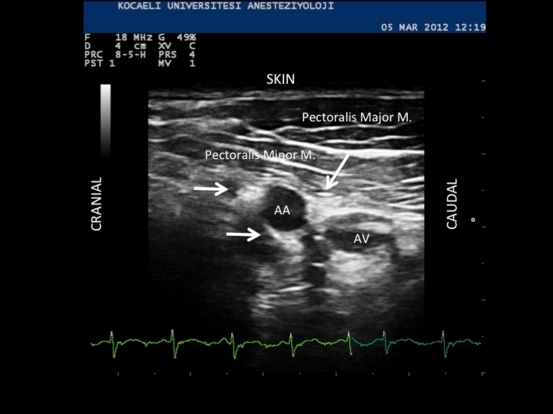
Figure 1. AA: Axillary (subclavian) artery, AV: Axillary vein. Cords of the brachial plexus appear hyperechoic. Arrows indicate lateral, posterior and medial cords. The axillary vein can be compressed to some extent.
The patient is placed in supine position with relaxed shoulders. Typically the arm to be blocked is adducted and the hand is on the abdomen but special arm positioning is not necessary, which is an advantage, especially in the case of painful, traumatized extremities. However, abduction of the arm will further bring cords to a more superficial position, which may be an advantage during deep blocks.[15] The head is rotated slightly to the opposite direction. The anesthesiologist works from behind the shoulder. The point of needle insertion is at the intersection between the clavicle and the coracoid process. The US probe is placed just below the clavicle, in para-sagittal orientation, about 0.5–1 cm inferior to the site of needle entry (Fig. 2). Any US machine with a variable frequency linear probe can be used for performing the block. In very obese patients, convex or microconvex probes should be considered.
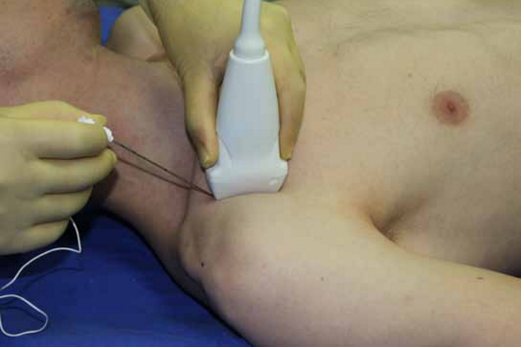
Figure 2. The point of needle insertion is at the intersection between the clavicle and the coracoid process. A linear probe is placed just below the clavicle inferior to the site of needle entry. Needle is directed using in-plane technique.
A 22 gauge, 80 mm block needle is used during block performance. The needle is directed in-plane with the US probe, and aimed towards the cranioposterior part of the axillary artery. The needle tip is positioned close to the recognizable cords around the 8 o’clock position based on a previous-published MRI study.1 The visualized local anesthetic (LA) distribution should be considered sufficient when it reaches all identified cords or surrounds the artery ina U shape covering 3–11 o’clock of the clock face. If spread is judged insufficient, the needle should be redirected to provide a U-shaped LA distribution around the axillary artery. In adult patients, we typically administer 30 ml of LA mixture (20 ml of levobupivacaine 0.5% and 10 ml of lidocaine 2%). If bilateral block is planned, we administer only 20 ml of LA for each side.
Single- versus Dual-Control during US-Guided ICB
Some clinicians choose to use both localization modalities, NS and US guidance, simultaneously for the performance of this block. However, avoidance of NS may result in a greater degree of patient comfort, especially in trauma cases, where motor stimulation may be quite painful. In a randomized study, it was shown that during LSIB performance, US guidance alone produces a block success rate identical to the combination of both US and NS guidance, yet provides a shorter block performance time.[16] Block onset time was similar in both groups. The axillary artery is a large, pulsatile landmark that can be easily identified during US scanning (Fig. 1). For these reasons, we recommend using US guidance alone.
ICB in Children
LSIB is easy to perform in children due to distinct anatomical landmarks. Using NS in our study that included 80 children, all patients received 0.5 mL kg-1 of bupivacaine 0.25% with adrenaline 5 mg mL-1. All of the patients were pain-free at awakening from general anesthesia with a mean duration of analgesia of 13 ± 8 h and a mean duration of motor block of 6 ± 2 h. Vascular puncture was detected in six patients.[17] Currently in our clinic, all ICB blocks in children are performed using US guidance alone and 0.25% levobupivacaine 0.5 ml.kg.
Possible complications
Vascular puncture with or without inadvertent LA toxicity is the most frequent complication described, although US guidance has dramatically reduced the incidence of this occurrence. Because ICB block is a relatively deep block, a noncompressible area, coagulopathy can be considered as a relative contraindication. Pneumothorax is probably the most feared complication; attention should be paid to stay strictly lateral and sagittal to avoid meeting the pleura.[18]
Catheter Technique
The infraclavicular area is the best site of the brachial plexus for catheter placement. Pectoral muscles keep the catheter in place, and therefore catheter dislodgment is not a major problem. Catheters are most useful for repeated surgery, daily debridement and painful complex surgeries like elbow surgery. During catheter placement we administer 20 ml of LA as described before. The needle tip is placed around 8 o’clock, and the catheter is further threaded about 2-3 cm beyond the tip of the needle. Different regimens (LA administration on demand, and/or continuous infusion via patient-controlled analgesia pumps) using dilute LA concentration can be used for pain treatment. We typically administer levobupivacaine 0.125-0.25% either 5 ml continuous infusion or 5 ml bolus doses on demand. All patients with catheters are followed at regular intervals and necessary adjustments should be made to optimize pain therapy and also to assess possible complications like infection, migration of the catheter, failure, and persistent motor or sensory block.
References
- Sauter AR, Smith HJ, Stubhaug A, et al. Use of magnetic resonance imaging to define the anatomical location closest to all three cords of the infraclavicular brachial plexus. Anesth Analg 2006; 103: 1574-1576.
- Bazy L. L’Anesthesie du plexus brachial. In: Pauchet V, Sourdat P, Laboure´ J, eds. L’Anesthesie regionale. Paris: Doin et Cie, 1917: 222–5.
- Raj PP, Montgomery SJ, Nettles D, Jenkins MT. Infraclavicular brachial plexus block – A new approach. Anesth Analg 1973; 52: 897-904.
- Klaastad Ø, Smith HJ, Smedby O, et al. A novel infraclavicular brachial plexus block: The lateral and sagittal technique, developed by Magnetic Resonance Imaging studies. Anesth Analg 2004; 98: 252-256.
- Koscielniak-Nielsen ZJ, Rasmussen H, Hesselbjerg L, et al. Infraclavicular block causes less discomfort than axillary block in ambulatory patients. Acta Anaesthesiol Scand. 2005; 49: 1030-1034.
- Klaastad O, Dodgson MS, Stubhaug A, Sauter AR. Lateral sagittal infraclavicular block (LSIB). Reg Anesth Pain Med. 2006; 31:86.
- Gürkan Y, Hosten T, Solak M, Toker K. Lateral sagittal infraclavicular block: clinical experience in 380 patients. Acta Anaesthesiol Scand. 2008; 52: 262-266.
- Koscielniak-Nielsen ZJ, Rasmussen H, Hesselbjerg L, et al. Clinical evaluation of the lateral sagittal infraclavicular block developed by MRI studies. Reg Anesth Pain Med. 2005; 30: 329-334.
- Sandhu NS, Capan LM. Ultrasound-guided infraclavicular brachial plexus block. BJA 2002; 89: 254-259.
- Sauter AR, Dodgson MS, Stubhaug A, et al. Electrical nerve stimulation or ultrasound guidance for lateral sagittal infraclavicular blocks: a randomized, controlled, observer-blinded, comparative study. Anesth Analg. 2008; 106: 1910-1915.
- Gürkan Y, Acar S, Solak M, Toker K. Comparison of nerve stimulation vs. ultrasound-guided lateral sagittal infraclavicular block. Acta Anaesthesiol Scand. 2008; 52: 851-855.
- Kus A, Gürkan Y, Gök CN, Solak M, Toker K. Infraclavicular block with ultrasound at amputated upper extremity. Agri. 2010; 22: 134-6.
- Tekin M, Gürkan Y, Ceylan DB, Solak M, Toker K.Ultrasound- guided bilateral infraclavicular block: case report Agri. 2010; 22: 41-3.
- Gürkan Y, Ozdamar D, Hosten T, Solak M, Toker K. Ultrasound guided lateral sagittal infraclavicular block for pectoral flap release. Agri. 2009; 21: 39-42.
- Bigeleisen P, Wilson M. A comparison of two techniques for ultrasound guided infraclavicular block. British Journal of Anaesthesia 2006; 96: 502–7.
- Gürkan Y, Tekin M, Acar S, Solak M, Toker K. Is nerve stimulation needed during an ultrasound-guided lateral sagittal infraclavicular block? Acta Anaesthesiol Scand. 2010; 54: 403-7.
- Gürkan Y, Ozdamar D, Solak M, Toker K. Lateral sagittal infraclavicular block is a clinically effective block in children. Eur J Anaesthesiol. 2008; 25: 949-951.
- Koscielniak-Nielsen ZJ, Rasmussen H, Hesselbjerg L. Pneumothorax after an ultrasound-guided lateral sagittal infraclavicular block. Acta Anaesthesiol Scand 2008; 52: 1176-7.
Leave a commentOrder by
Newest on top Oldest on top