FNB vs ACB: Anatomy, Tips, and Clinical Pearls
Note: This article originally appeared in the ASRA News, Volume 16, Issue 2, pp. 21-27 (May 2016).
In addition, ASRA's Regional Anesthesia and Pain Podcast ( ASRA RAPP) offered a lively discussion on this topic featuring some of the authors of this article.
Section Editor: Sarah Madison, MD
Introduction
Whether you embrace the versatility of the adductor canal block (ACB) or maintain loyalty to the femoral nerve block (FNB), new knowledge and techniques are constantly emerging. We asked experts from around the world to tell us their approach.
Femoral Nerve Block
Stephen Choi BSc, MSc, MD, FRCPC
Assistant Professor, Department of Anesthesia
Director, Clinical Research Unit
Sunnybrook Health Sciences Centre
University of Toronto
Femoral nerve block (FNB) was described in 1952 where, in combination with sciatic nerve block, it was used for surgical anesthesia of the lower extremity.[1] Continuous and single injection FNB have been the mainstay of postoperative analgesia for surgical procedures on the anterior thigh, femur, or knee, particularly since ultrasound (US) guidance became commonplace. These procedures include total knee arthroplasty, ACL reconstruction, and procedures on the mid-to-distal femoral shaft and patella. Meta-analysis of randomized trials has confirmed that FNB provides superior analgesia and reduces opioid consumption in comparison to systemic analgesia alone.[2] The potential drawbacks include quadriceps weakness that, in the absence of proper preventive measures, can potentially delay postoperative mobilization and/or increase the risk of falls.
Currently, FNB is being compared to adductor canal block (ACB) and periarticular infiltration (LIA)—both of which can better preserve quadriceps strength—for total knee arthroplasty. Several reports have demonstrated earlier ambulation with these newer techniques, though no difference in time to readiness to discharge; and no studies have demonstrated superior long-term functional outcomes.[3] In terms of analgesic efficacy, studies have failed to demonstrate any differences between ACB, LIA, and/or FNB (although these were not specifically designed to examine analgesic equivalence).[4,5] The one trial appropriately powered to make analgesic comparisons between cFNB and cACB is limited by a study design that includes patient-controlled epidural analgesia (PCEA) administered concurrently with the peripheral nerve blocks.[6]
Anatomy and Technique
The femoral nerve, a branch of lumbar plexus (L2,3,4), lies lateral to the femoral artery, deep to the fascia iliaca, and superficial to the iliopsoas muscle. The posterior division gives sensory articular branches to the knee joint and motor branches to the quadriceps before terminating as the saphenous nerve.
The sono-anatomy is straightforward, and single-injection FNB is considered a basic technique. In classical teaching, FNB is performed proximal to the branching of profunda femoris from the femoral artery. This is usually just distal to the inguinal ligament. A common error is to mistake the inguinal crease of the surface anatomy as equivalent to the inguinal ligament when the ligament is in fact proximal to the crease. US imaging can clearly identify the nerve, lateral to the artery, deep to the fascia iliaca, and superficial to the iliopsoas muscle. Beware of lymph nodes that can have similar echogenicity as the nerve. A proximal and distal site survey will allow easy differentiation between lymph nodes and nerve tissue.
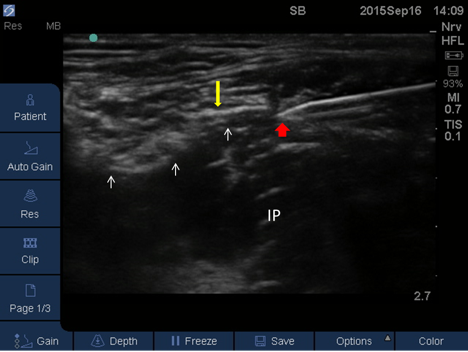
Figure 1. Femoral nerve block. Red arrow: needle tip; yellow arrow: fascia iliaca; white arrows: femoral nerve; IP: iliopsoas muscle.
Tips and Pearls
For an in-plane approach using short-axis imaging, the decision to use peripheral nerve stimulation (PNS) is at the discretion of the clinician. For the out-of-plane short axis approach, use PNS and maintain stimulation as the catheter is threaded. My preferred technique is in-plane, without PNS, and I thread the catheter under direct US vision through the needle and place the catheter tip deep to the nerve (Figures 1 and 2). I advance the catheter with my index finger and thumb while holding the needle between my fourth and fifth finger of the same hand (Figure 3). I find that this allows me the maximum flexibility to place the catheter tip as desired. I do not advocate threading the catheter a standard distance blindly as one cannot control the final position of the catheter tip in relation to the nerve. This can result in secondary catheter failure because a large volume bolus of local anesthetic will bathe the nerve but a low rate infusion with dilute concentration may not spread back to the nerve (Figure 4). My local anesthetic selection: Initial bolus of 10-20 mL of ropivacaine 0.5% followed by an infusion of ropivacaine 0.15% at 5 mL/h with catheter removal on the second postoperative day at 06:00.
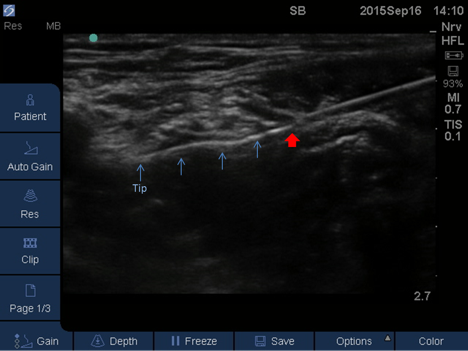 Figure 2. Femoral nerve block. Red arrow: needle tip; blue arrows: perineural catheter advancing out of needle
Figure 2. Femoral nerve block. Red arrow: needle tip; blue arrows: perineural catheter advancing out of needle
At our institution, we use cFNB with multimodal analgesia for total knee arthroplasty (TKA). A knee brace is utilized while the cFNB is in situ. Nerve blocks and spinals are performed in a separate block room to allow for minimal turnover time between cases. Because a tourniquet is routinely used on the mid to upper thigh, we do not use ACB catheters (concerns over nerve compression). Our experience with cFNB is that it functions well: patients have excellent analgesia, with the vast majority of patients achieving home discharge criteria by postoperative day 3.
With a comprehensive falls prevention program, the incidence of falls after TKA is <0.5% at our institution (internal quality data), well below the published rate of falls (1.6%) in patients undergoing TKA with or without nerve blocks.[7] The relative merits of ACB versus FNB on immediate postoperative milestones depend on the duration of infusion and concentration of local anesthetic. In the setting of hospital admission, we select FNB.
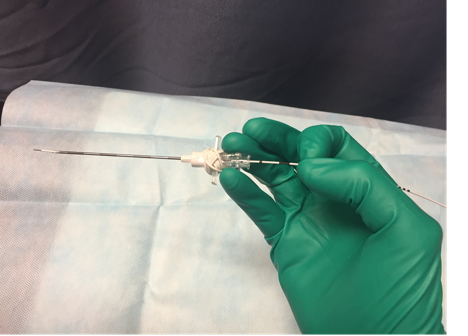 Figure 3. Stabilize the needle with fourth and fifth digits. Advance the catheter under direct ultrasound guidance with first and second digits
Figure 3. Stabilize the needle with fourth and fifth digits. Advance the catheter under direct ultrasound guidance with first and second digits
In my opinion, the literature is still unclear as to the analgesic equivalency of ACB versus FNB. While the ACB—when performed properly—preserves quadriceps function compared to FNB, and can provide good analgesia for the antero-medial aspect of the knee, it does not provide reliable analgesia to the anterior parts of the knee (cutaneous included).
For all these reasons, we have elected to continue with post-TKA analgesia using cFNB, opioids, and opioid-sparing adjuncts like acetaminophen and non-steroidal anti-inflammatory drugs (NSAIDs). Additional adjuncts, if necessary, include pregabalin, nabilone, and ketamine. For patients with chronic pain or opioid tolerance we also use a continuous sciatic nerve block. ACB has its place in our practice for ambulatory patients in whom motor weakness must be minimized, but for TKA we await conclusive evidence of superiority before changing what has worked well in our practice.
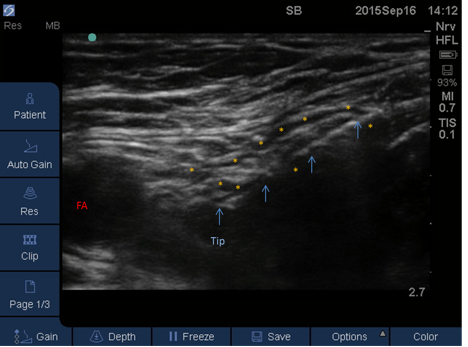 Figure 4. Femoral nerve block. Blue arrows: perineural catheter; asterisks: local anesthetic surrounding the femoral nerve; FA: femoral artery
Figure 4. Femoral nerve block. Blue arrows: perineural catheter; asterisks: local anesthetic surrounding the femoral nerve; FA: femoral artery
Adductor Canal Block
Anthony T. Machi, MD
Assistant Professor
Department of Anesthesiology and Pain Management
UT Southwestern Medical Center, Dallas
Anatomy
The adductor canal is a musculo-aponeurotic tunnel in the lower one-third of the thigh. It contains the saphenous nerve, motor nerve to the vastus medialis, femoral artery, and femoral vein, and it may also contain the posterior obturator nerve, other cutaneous sensory nerves originating from the femoral nerve, and perforating arteries and veins. Prior to entering the canal, these structures traverse the femoral triangle with the exception of the posterior obturator. While in the femoral triangle, the femoral nerve arborizes into its terminal branches such that the saphenous nerve, motor nerve to the vastus medialis, and possibly other terminal branches destined for sensation of the distal medial thigh course together as they abut the femoral artery and vein and are invested by connective tissue. Together, these structures travel toward the distal thigh. In the lower one-third of the thigh, the vastoadductor membrane originates from connective tissue contiguous with the adductor magnus, and extends toward the vastus medialis deep to the sartorius.[8] This membrane forms a roof for the neurovascular structures, separating them from the muscles nearby: sartorius, vastus medialis and adductor longis.[9,10] The length of the canal varies from 5.5 to 15 cm while the width varies from 2.2 cm proximally to 0.5 cm distally.[8] The distance of the proximal aspect of the canal relative to the anterior superior iliac spine (ASIS) is a mean of 28 cm with a range of 20- 32 cm. The neurovascular bundle is dynamic. It twists slightly upon itself as it travels through the thigh such that the relative position of each of these structures to each other changes when viewed in a transverse short-axis plane along a cephalad-caudad axis. These anatomic relationships and depictions have been previously published.[11]
Ultrasound Technique
The method described by Lund[12], Jenstrup[13] and Jaeger[14] is a well-validated method for performing the adductor canal block (ACB) and a basis for how the block may be performed.[15] The patient is placed in the supine position and instructed to allow the leg to externally rotate at the hip to comfort with a slight bend in the knee if necessary to aid in attaining this position. The mid point is measured and identified between the ASIS and the cephalad margin of the patella. A high-frequency linear array ultrasound probe is then placed at this mid point on the anteromedial aspect of the thigh. The superficial femoral artery is identified typically at a depth of 2-4 cm. In a short-axis view, it may be visualized deep to the subcutaneous fat and sartorius muscle, medial to the vastus medialis (or on occasion the rectus femoris), and anterior to the adductor longis muscle, with the femoral vein usually posterolateral to the artery (Figures 5A and 5B). The position of the femoral vein may vary relative to the artery at this level of the thigh (Figures 6A and 6B).
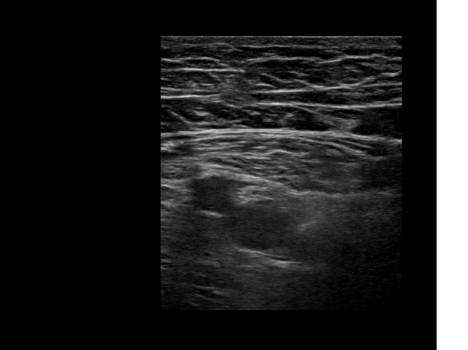 | 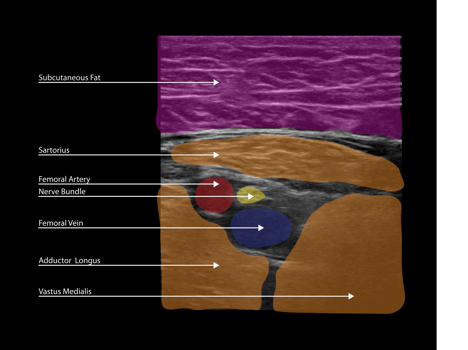 |
Figure 5. Adductor canal block. A: This is the most common view of the anteromedial thigh at the mid point between the ASIS and the cephalad margin of the patella. B: Color has been added to highlight important anatomical structures
At this position, the ultrasound image of the saphenous nerve or nerve bundle is typically anterolateral to the superficial femoral artery within the adductor canal. The corresponding sonoanatomical positions for each structure are: saphenous nerve anterior to the artery, vein lateral to the artery, and sartorius muscle medial to the artery (Figures 5A and 5B).[16,17] Though the great majority of individuals have these structures oriented as such, it is possible to encounter the nerve bundle anteromedial or medial to the artery.
This location is then evaluated for the adequacy of needle placement, as there may be a perforating vein or even a perforating artery visualized. If necessary, the thigh is scanned distally along the canal to find a suitable location to perform the block. Performing the procedure proximal from the midpoint is avoided, as this would more likely produce a block higher in the femoral triangle, increasing the likelihood of local anesthetic spread to the other motor branches of the femoral nerve. The block may be performed distally in the caudad portion of the canal, but proximal to the adductor hiatus. The hiatus is noted where the femoral artery courses deep and moves away from the anterior muscle plane (sartorius and vastus medialis muscles), toward the posterior aspect of the thigh where it becomes the popliteal artery. The most distal suitable location for the block is 2-3 cm cephalad from the hiatus.[9]
Once the desired location is identified, a needle is then inserted in-plane from the anterolateral side of the transducer, through the sartorius or vastus medialis muscle with the final needle tip position resting adjacent to the artery and deep to the saphenous nerve (Figures 7A and 7B).
 | 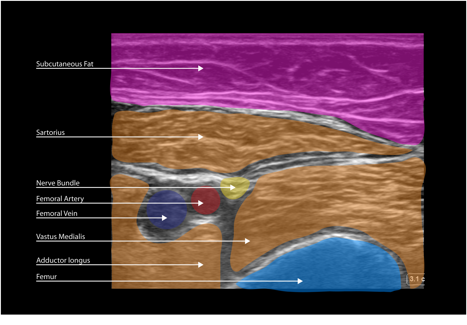 |
Figure 6. Adductor canal block. A: This is a variant in a different, thin patient at the mid point of the ASIS and the cephalad margin of the patella. The femoral vein is observed posteromedial to the artery rather than the more common position, posterolateral to the artery. B: Color has been added to highlight important anatomical structures.
For a single injection block 10-20 mL of injectate is deposited in increments.
Advantages and Disadvantages
A critique of this technique is that the starting point described may not be within the adductor canal proper but rather the distal femoral triangle.[18,19] In contrast, others report that the subsartorial fascial plane is contiguous with the vastoadductor membrane, allowing for spread of injectate from a point within the distal femoral triangle into the adductor canal.[20-22] My own observations are consistent with those of Jaeger, Cowlishaw, and others in that blockade primarily of the saphenous nerve with the aforementioned technique provides reliable and effective analgesia of the medial-anterior knee and medial thigh as a single injection or continuous technique. Though injectate may spread in either a caudad or cephalad direction, it may often be visualized filling the space within the vastoadductor membrane and rarely travels cephalad so far as to anesthetize the other motor branches of the femoral nerve (though this is possible).[23]
Whether this slightly more proximal position affects the nature of the block is debated in the literature. In my experience, there is no appreciable clinical difference in the analgesia provided or strength and function of the leg between the two positions.
In addition, performing the block as cephalad as the midpoint from the ASIS to the cephalad margin of the patella allows for a greater distance from the surgical field so that a perineural catheter placed there can be outside of the surgical field.
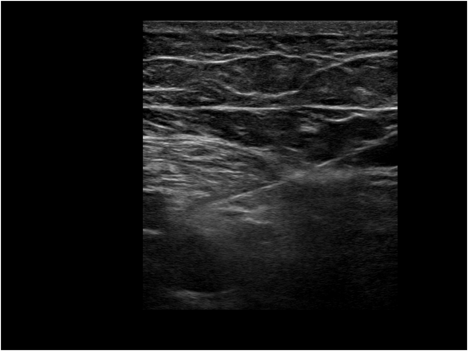 |  |
Figure 7. Adductor canal block. A: This is the same patient and position as Figure 5 with a 21 GA short bevel needle placed as described, prior to injection. B: Color has been added to highlight important anatomical structures.
My selection of ACB or FNB is based on the type of surgery and underlying patient characteristics. Three of the most important sets of questions are:
- Is it a primary or revision TKA?
- Is a chronic pain condition present? Is the patient taking opioids chronically and exhibiting opioid tolerance?
- What is the time to the first anticipated physical therapy session?
Short-term physical therapy goals for hospital discharge following TKA include independent transfers, functional mobilization, and ambulation permitting basic activities of daily living.[24],[25] ACB has been shown to greatly improve quadriceps strength and function relative to FNB.[26] Moreover, ACB has been shown to greatly facilitate ambulation and successful physical therapy following TKA relative to FNB. [15],[27],[28]
Most patients will benefit from LIA of the posterior capsule and deep lateral tissues of the knee in addition to the perineural blockade. Dose adjustment for the local anesthetic for infiltration is made based on the weight, age, and comorbid conditions of the patient to reduce the risk of local anesthetic systemic toxicity.
There is a subset of patients undergoing TKA who still have severe pain despite a functional FNB. This may originate from the sciatic or possibly obturator distributions. The same is true for patients who have ACB. The knee is innervated by multiple nerves, and without blocking all of them, some patients may exhibit severe pain. For this reason, I advocate a multimodal approach including LIA, and ACB or FNB are anchors to the analgesic regimen. In my experience, patients undergoing revision TKA and who have chronic pain and opioid tolerance are better candidates for FNB.
Tips and Pearls
If there is any question as to the position of the nerve bundle, one may identify the femoral nerve cephalad in the femoral triangle prior to its arborization and scan along its length to the desired position of blockade in the distal thigh.
When the canal is located more than 4 cm deep, it is often helpful to use a large gauge needle such as a 17GA Tuohy for its rigidity and ease of imaging.
A sonoanatomical mark of successful needle tip placement is circular enlargement of the vastoadductor membrane around the nerve bundle. Injectate deposited deep to the sartorius but not within the canal will appear more ellipsoid.
When placing a perineural catheter, the catheter tip should be visualized adjacent to the nerve bundle within the canal.
There is often a tactile component to successful needle placement; a small “pop” or release of tissue may be appreciated as the adductor canal is entered.
Adductor Canal Block
Pia Jæger, MD, PhD
Department of Anaesthesia, Centre of Head and Orthopaedics,
Copenhagen University Hospital, Rigshospitalet,
Copenhagen, Denmark
Ulrik Grevstad, MD
Department of Anaesthesia and Intensive Care Medicine,
Copenhagen University Hospital, Gentofte Hospital
Also Copenhagen? Denmark
Due to its effect on quadriceps strength, and thereby a potential delay in mobilization, we pretty much abandoned the FNB for knee surgery or surgery in the lower limb almost a decade ago. The void following the virtual extinction of the FNB had us looking for alternative methods, leading us to the ACB.
Ultrasound Technique
In our group, we perform the ACB at the midthigh level using a subsartorial approach. We position the patient in the supine position with the leg to be blocked slightly externally rotated. Using a high-frequency linear array ultrasound transducer, we perform a dynamic survey of the medial part of the midthigh in a short-axis view. We start the survey by positioning the transducer approximately halfway between the anterior superior iliac spine and the patella. First, we identify the superficial femoral artery deep to the sartorius muscle. At this level, the femoral vein is usually seen underneath the artery in the ultrasound image. After identifying the artery, we move the transducer cephalad and caudad along the artery to determine the best site for visualization of the saphenous nerve adjacent to the superficial femoral artery in the adductor canal. Although not always distinctly visualized, the saphenous nerve lies anterolateral to the artery at this level and can usually be seen at the junction between the artery, sartorius muscle, and vastus medialis muscle.
Single-shot injections
For single-shot injections, we use an in-plane technique. We insert an 80-mm needle in-plane with the transducer in an anterolateral to posteromedial direction. When advancing the needle, we avoid the fascial plane between the vastus medialis muscle and the sartorius muscle, as the nerve to the vastus medialis can be found in this plane.[29] If not visualized prior to the deposition of local anesthetic, the saphenous nerve often becomes visible after the injection. We deposit the local anesthetic in proximity of the saphenous nerve, anterolateral to the superficial femoral artery. While injecting the local anesthetic we move the transducer in a cephalad-to-caudad direction to ensure proper spread within the canal.
Continuous catheters
For continuous catheters, we have recently changed our procedure to an out-of-plane technique. We start out by performing an ultrasound survey identical to that for the single-shot blocks. After having identified the target site, we move the transducer proximally, a few centimeters further than the depth of the target site, and insert the needle out-of-plane in a cephalad-to-caudad direction. Under ultrasound guidance, we advance the needle at a 45-degree angle, reaching the target slightly proximal to the midthigh level. After ensuring correct placement of the needle tip, we expand the canal using approximately 10 ml of local anesthetic to ease advancement of the catheter. We then advance the catheter approximately 5 cm beyond the tip of the needle. Thus, the catheter tip will be positioned approximately at the midthigh level. After removal of the needle, correct position of the catheter is confirmed by injecting 10–20 mL of local anesthetic through the catheter. In lean patients, it is almost always possible to visualize the catheter in long axis view. Color flow or power doppler may be helpful for visualizing injectate spread in obese patients. By placing the catheter along the neurovascular bundle for some distance, we hope to see less displacement of our catheters.
Tips and Pearls
Nowadays, we almost exclusively perform ACBs for knee surgery and saphenous blocks (smaller volume) for surgery below the knee. We only consider the FNB in the rare cases where we cannot place an ACB (e.g., some extremely obese patients).
We have become increasingly aware of the different fascia layers in the adductor canal and their influence in placing a successful ACB. A cadaver study by Andersen[29] showed that the roof of the adductor canal is made by a continuous, unbroken thin fascia (a proximal extension of the thicker vastoadductor membrane). This fascia extends in the entire length of the adductor canal, just deep to the sartorius muscle. Failure to get underneath this fascia leads to a spread of local anesthetic within the subsartorial fat compartment. This can be seen as a distinct “flat spread” that lifts the sartorius muscle away from the adductor canal, whereas spread within the adductor canal goes deeper between the vastus medialis and the superficial femoral artery. Spread within the subsartorial fat compartment can initially mimic spread within the adductor canal, especially in very obese patients. Most likely, the saphenous nerve will still be affected by simple diffusion but other nerves traversing the adductor canal will probably not, potentially resulting in inferior analgesia. Because the saphenous nerve will be affected in either case, it is difficult to differentiate whether inadequate analgesia is caused by a misplaced block (in the subsartorial compartment) or whether the pain originates from areas innervated by other nerves such as the sciatic nerve.
We recommend using 20–30 ml of local anesthetic for an ACB. According to the anatomy, four nerves pass through the adductor canal: the saphenous nerve, the nerve to the vastus medialis, the medial femoral cutaneous nerve, and the posterior branch of the obturator nerve. In theory, the ideal volume for an ACB will ensure sufficient spread to all nerves within the adductor canal without any major motor involvement. In a recent study,[30] we have shown that the smallest effective volume ensuring distal filling of the adductor canal is 20 mL of local anesthetic, thus potentiating a block of the terminal end of the obturator nerve. In another study using EMG recordings,[31] we found that the nerve to the vastus medialis was anesthetized in 35%, 84%, and 100% of subjects following an ACB with 10, 20, and 30 mL of local anesthetic, respectively. Only two subjects had a concurrent affection of the vastus lateralis muscle; one subject after an ACB with 20 mL of local anesthetic, another after receiving an ACB with 30 mL. In neither of the two studies was there an association between volume and quadriceps muscle strength, and, most importantly, the overall effect on quadriceps strength was modest, which has also been shown in other studies.[32-34] These results indicate that higher volumes of local anesthetic may improve the analgesic effect of an ACB without increasing adverse motor effects from the block, but this needs to be confirmed in a clinical setting, powered not only to show differences in analgesic efficacy, but also in adverse events.
Regarding continuous infusions, we have had good experience using an infusion rate of 8 ml/h of 0.2% ropivacaine. However, it is worth noting that we initially chose this regimen to ensure that the total dosing over time equaled that of the single injections. Currently, we are conducting a study comparing the analgesic effect of intermittent boluses with continuous infusions via a catheter. Our hypothesis is that a certain volume is needed to ensure blocking of all the nerves passing through the canal and that this may be more consistently obtained by intermittent boluses. The results of this study will guide our way for subsequent studies optimizing the catheter-based regimens for ACBs.
References
- Moore DC. Sciatic and femoral nerve block. J Am Med Assoc. 1952;150:550-4.
- Paul JE, Arya A, Hurlburt L, et al.. Femoral nerve block improves analgesia outcomes after total knee arthroplasty: A meta-analysis of randomized controlled trials. 2010; 113:1144-62.
- Perlas A, Kirkham KR, Billing R, et al. . The impact of analgesic modality on early ambulation following total knee arthroplasty. Reg Anesth Pain Med. 2013; 38:334-9.
- Grevstad U, Mathiesen O, Valentiner LS, Jaeger P, Hilsted KL, Dahl JB. Effect of adductor canal block versus femoral nerve block on quadriceps strength, mobilization, and pain after total knee arthroplasty: A randomized, blinded study. Reg Anesth Pain Med. 2015; 40:3-10.
- Jaeger P, Zaric D, Fomsgaard JS, et al. Adductor canal block versus femoral nerve block for analgesia after total knee arthroplasty: A randomized, double-blind study. Reg Anesth Pain Med. 2013; 38:526-32.
- Kim DH, Lin Y, Goytizolo EA, et al. Adductor canal block versus femoral nerve block for total knee arthroplasty: A prospective, randomized, controlled trial. 2014; 120:540-50.
- Memtsoudis SG, Danninger T, Rasul R, et al.. Inpatient falls after total knee arthroplasty: The role of anesthesia type and peripheral nerve blocks. 2014; 120:551-63.
- Tubbs RS, Loukas M, Shoja MM, Apaydin N, Oakes WJ, Salter EG. Anatomy and potential clinical signifiance of the vastoadductor membrane. Surg Radio Anat. 2007; 29:569-73.
- Manickam B, Perlas A, Duggan E, Brull R, Chan VW, Ramlogan R. Feasibility and efficacy of ultrasound-guided block of the saphenous nerve in the adductor canal. Reg Anesth Pain Med. 2009; 34:578-80.
- Davis JJ, Bond TS, Swenson JD. Adductor canal block: More than just the saphenous nerve? Reg Anesth Pain Med. 2009; 34:618-9.
- Bendtsen TF, Moriggl B, Chan V, Borglum J. Basic topography of the saphenous nerve in the femoral triangle and the adductor canal. Reg Anesth Pain Med. 2015; 40:391-2.
- Lund J, Jenstrup MT, Jaeger P, Sorensen AM, Dahl JB. Continuous adductor-canal-blockade for adjuvant post-operative analgesia after major knee surgery: Preliminary results. Acta Anaesthesiolog Scand. 2011; 55:14-9.
- Jenstrup MT, Jaeger P, Lund J, et al. Effects of adductor-canal-blockade on pain and ambulation after total knee arthroplasty: A randomized study. Acta Anaesthesiolog Scand. 2012; 56:357-64.
- Jæger P, Grevstad U, Henningsen MH, Gottschau B, Mathiesen O, Dahl JB. Effect of adductor-canal-blockade on established, severe post-operative pain after total knee arthroplasty: A randomised study. Acta Anaesthesiolog Scand. 2012; 56:1013-9.
- Machi AT, Sztain JF, Kormylo NJ, Madison SJ, Abramson WB, Monahan AM, et al. Discharge readiness after tricompartment knee arthroplasty: Adductor canal versus femoral continuous nerve blocks-A dual-center, randomized trial. 2015; 123:444-56.
- Weller RS, Henshaw DS. The use of anatomical position for regional block description. Reg Anesth Pain Med. 2014; 39:263-4.
- Jæger P, Zaric D, Koscielniak-Nielsen ZJ, Dahl JB. Reply to Drs Weller and Henshaw. Reg Anesth Pain Med. 2014; 39:264.
- Bendtsen TF, Moriggl B, Chan V, Pedersen EM, Borglum J. Defining adductor canal block. Reg Anesth Pain Med. 2014; 39:253-4.
- Bendtsen TF, Moriggl B, Chan V, Pedersen EM, Børglum J. Redefining the adductor canal block. Reg Anesth Pain Med. 2014; 39:442-3.
- Cowlishaw P, Kotze P. Adductor canal block--or subsartorial canal block? Reg Anesth Pain Med. 2015; 40:175-6.
- Cowlishaw P, Kotze P. Reply to Dr Bendtsen. Reg Anesth Pain Med. 2015; 40:392-3.
- Yuan SC, Hanson NA, Auyong DB, Choi DS, Coy D, Strodtbeck WM. Fluoroscopic evaluation of contrast distribution within the adductor canal. Reg Anesth Pain Med. 2015; 40:154-157.
- Chen J, Lesser JB, Hadzic A, Reiss W, Resta-Flarer F. Adductor canal block can result in motor block of the quadriceps muscle. Reg Anesth Pain Med. 2014; 39:170-1.
- Artz N, Elvers K, Lowe CM, Sackley C, Jepson P, Beswick AD. Effectiveness of physiotherapy exercise following total knee replacement: Systematic review and meta-analysis. BMC Musculoskeletal Disorders. 2015; 16:15.
- Husted H, Lunn TH, Gaarn-Larsen L, Kristensen BB, Kehlet H. Why still in hospital after fast-track hip and knee arthroplasty? Acta Orthopaedica. 2011; 82:679–684.
- Jaeger P, Nielsen ZJ, Henningsen MH, Hilsted KL, Mathiesen O, Dahl JB. Adductor canal block versus femoral nerve block and quadriceps strength: A randomized, double-blind, placebo-controlled, crossover study in healthy volunteers. 2013; 118:409-15.
- Grevstad U, Mathiesen O, Valentiner LS, Jaeger P, Hilsted KL, Dahl JB. Effect of adductor canal block versus femoral nerve block on quadriceps strength, mobilization, and pain after total knee arthroplasty: A randomized, blinded study. Reg Anesth Pain Med. 2015; 40:3–10.
- Perlas A, Kirkham KR, Billing R, et al. The impact of analgesic modality on early ambulation following total knee arthroplasty. Reg Anesth Pain Med. 2013; 38:334–339.
- Andersen HL, Andersen SL, Tranum-Jensen J. The spread of injectate during saphenous nerve block at the addutor canal: A cadaver study. Acta Anaesthesiol Scand. 2015; 59:238-45.
- Jæger P, Jenstrup MT, Lund J, et al. Optimal volume of local anaesthetic for the adductor canal block – using the continual reassessment method to estimate the ED95. Br J Anaesth. 2015; 115:920-6.
- Grevstad U, Jæger P, Sørensen JK, et al. Effect of local anesthetic volume within the adductor canal on quadriceps femoris function evaluated by electromyography: A randomized, observer- and subject-blinded, placebo-controlled study in volunteers. Submitted to Anesth Analg.
- Jæger P, Nielsen ZJ, Henningsen MH, Hilsted KL, Mathiesen O, Dahl JB. Adductor canal block versus femoral nerve block and quadriceps strength: A randomized, double-blind, placebo-controlled, crossover study in healthy volunteers. 2013; 118:409-15.
- Kwofie MK, Shastri UD, Gadsden JC, et al. The effects of ultrasound-guided adductor canal block versus femoral nerve block on quadriceps strength and fall risk: A blinded, randomized trial of volunteers. Reg Anesth Pain Med. 2013; 38:321-5.
- Jæger P, Koscielniak-Nielsen ZJ, Hilsted KL, Fabritius ML, Dahl JB. Adductor canal block with 10 mL versus 30 mL local anesthetics and quadriceps strength: A paired, blinded, randomized study in healthy volunteers. Reg Anesth Pain Med. 2015; 40:553-8.
Leave a commentOrder by
Newest on top Oldest on top