How I Do It: Ultrasound-Guided Injection for the Shoulder (Part 1)
This article originally appeared in ASRA News, Volume 13, Number 2, pp 6-9 (February 2013).
Author
Philip Peng, MBBS, FRCPC Founder (Pain Medicine)
Department of Anesthesia and Pain Management
University Health Network and Mount Sinai Hospital
University of Toronto
Toronto, Canada
Section Editor: David Provenzano, MD
Shoulder pain is very common in the general population. It has been estimated that one in five individuals will suffer shoulder pain during his/her lifetime.[1] It is responsible for 16% of all musculoskeletal complaints in the primary care setting[2] and is only second to low back pain as the most common musculoskeletal ailment in general practice.[3]
In most patients, chronic shoulder disorder can initially be managed conservatively with multimodal therapy consisting of activity modification, physical therapy, medications, and corticosteroid injections.[4] This two-part series will describe ultrasound-guided injections for the long head of biceps tendon (LHB), acromioclavicular joint (ACJ), subacromial subdeltoid bursa, and glenohumeral joint with LHB and ACJ injections covered in this article. A comprehensive review has recently been published on this subject for reference.[5,6]
Long Head of Biceps Tendon
Anatomy
The proximal part of LHB tendon is intra-articular (extrasynovial) and arises from the supraglenoid tubercle and the superior labrum. The tendon exits the joint within the bicipital groove, where an extension of the synovial lining of the GHJ invests the LHB tendon down to approximately 3-4 cm beyond the distal end of the groove. The LHB tendon is covered by the transverse humeral ligament and accompanied by the ascending branch of the anterior circumflex artery. The rotator cuff interval (RCI) is a triangular space that occupies the area between the subscapularis (SSC) and supraspinatus (SS) tendons and the base of the coracoid process. It is a space where the GHJ synovial lining extends around the biceps tendon and where the arthroscope enters the GHJ to avoid damaging the cuff tendons. Thus, this is an entry site by which an interventional pain physician can access the GHJ (Figs. 1A,B). The RCI is roofed by the rotator interval capsule, which is principally made up of the coracohumeral ligament (CHL). The RCI contains the tendon of the LHB tendon and the superior glenohumeral ligament (SGHL).

 Figure 1. A) Anterosuperior view showing the rotator cuff interval, which is a triangular space between the tendons of subscapularis (anterior) and supraspinatus (posterior) muscles, and the base of the coracoid process. The roof is the coracohumeral ligament (ghosted) and the contents are the long head of biceps tendon (blue) and superior glenohumeral ligament (green). B) Cut out of the rotator cuff interval to show the content. The superior glenohumeral ligament (SGHL), a focal thickening of the glenohumeral joint capsule, runs anterior to the tendon of the long head of biceps (LHB) initially (position a). The SGHL maintains a close relationship with the LHB and subsequently inserts into a small depression above the lesser tuberosity (position b), contributing to the biceps reflection pulley (position c) to prevent the dislocation of the LHB. Reprinted with permission from http://usra.ca.
Figure 1. A) Anterosuperior view showing the rotator cuff interval, which is a triangular space between the tendons of subscapularis (anterior) and supraspinatus (posterior) muscles, and the base of the coracoid process. The roof is the coracohumeral ligament (ghosted) and the contents are the long head of biceps tendon (blue) and superior glenohumeral ligament (green). B) Cut out of the rotator cuff interval to show the content. The superior glenohumeral ligament (SGHL), a focal thickening of the glenohumeral joint capsule, runs anterior to the tendon of the long head of biceps (LHB) initially (position a). The SGHL maintains a close relationship with the LHB and subsequently inserts into a small depression above the lesser tuberosity (position b), contributing to the biceps reflection pulley (position c) to prevent the dislocation of the LHB. Reprinted with permission from http://usra.ca.
Sonoanatomy
The patient is positioned sitting with back support and the hand supinated (“Give me your money gesture”). Place a high frequency (6-13 MHz) linear ultrasound probe over the bicipital groove (surface landmark halfway between the clavicle and anterior axillary fold). The LHB is seen as either a hyperechoic or a hypoechoic structure (anisotropy) between the greater and lesser tuberosity covered by transverse humeral ligament (Figs. 2A,B). A Doppler scan is then performed to reveal the ascending branch of the anterior circumflex artery (Fig. 2C). Doppler may also reveal increased vascularity of the tendon due to inflammation.
Procedure
My preference is to use a 25 gauge 1.5 inch needle. The injectate is 2-4 mL of 0.25% bupivacaine including 20-40 mg methylprednisolone acetate and the approach is either in-plane or out-of-plane. The target is the synovial sheath. Thus a successful injection should reveal the injectate surrounding the tendon. If the tendon swells up during injection, injection should stop as it signifies intratendinous injection, and the needle should be repositioned.



Figure 2. A) Ultrasound image showing the presence of long head of bicep (LHB) tendon (*) within the bicipital groove. The insert shows the position of the patients and the linear ultrasound probe. Note that the LHB tendon appears hyperechoic. B) Ultrasound image similar to 2A with a different tilt of the ultrasound probe. It demonstrates anisotropy with the LHB tendon (*) changed from hyperechoic to hypoechoic. The insert shows the position of the probe and the corresponding anatomical structures underneath. C) Doppler scan shows the ascending branch of the anterior circumflex artery (A); LT=lesser tuberosity; LHB=long head of biceps. Reprinted with permission from http://usra.ca. |
Literature review
Primary tendinitis (in the absence of other shoulder pathology) is rare. Biceps tendon disease can be divided into tendinitis and tenosynovitis. The latter refers to an inflamed tendon sheath with the tendon in a relatively normal shape and is more responsive to non-operative management including steroid injection. However, tendinitis is more recalcitrant to conservative therapy.
To achieve maximum benefit, steroid should be injected into the tendon sheath only and intratendinous injection should be avoided. This injection is technically difficult to achieve with palpation only, and ultrasound guidance is a reasonable method for accurate injection. There is only one study comparing the ultrasound-guided and palpation method using CT scan as the validating tool.[7] All ultrasound-guided injections reached the tendon sheath but one-third of injections by palpation did not reach the tendon sheath. Correct placement of injectate results in better outcome. In a prospective randomized trial, ultrasound-guided injection resulted in greater improvement in pain score and Constant-Murley score (measuring pain, ADL, range and strength) over the palpation method.[8] The mean follow up time was 33 weeks (range 24 to 56 weeks). The visual analog scale score decreased from 7.1 ± 2.3 before injection to 4.2 ± 3.1 at follow-up with blind method and from 6.9 ± 2.6 to 2.1 ± 1.9 in the ultrasound-guided group (p <0.05). The Constant-Murley score improved from 31.4 ± 11.6 before injection to 73.5 ± 19.2 at follow-up and from 32.5 ± 14.7 to 85.5 ± 10.3 (p <0.01) in the palpation group and ultrasound–guided injection groups respectively. A total of 9 patients in the palpation group and 5 patients in the ultrasound guided injection groups were refractory to the steroid injections. Follow-up arthroscopy in patients refractory to treatment demonstrated severely frayed LHB tendons in 44% of the patients in blind injection group compared to 100% of the patients in the ultrasound-guided injection. Based on these findings the authors concluded that patients with intratendinous pathology were more recalcitrant to conservative treatment including corticosteroid injections.
Acromioclavicular Joint
The ACJ injection is commonly used as a diagnostic test to localize the source of pain in ACJ injury.[5,6] The main therapeutic indication for ACJ injection is arthritis (post-traumatic and osteoarthritis). Although the radiological evidence of osteoarthritis in ACJ is in the range of 50-60%, the prevalence of clinically symptomatic ACJ osteoarthritis is lower.[9] In contrast, arthritis following trauma to ACJ is more common due to the frequency of injury to this vulnerable joint.[10]
Anatomy

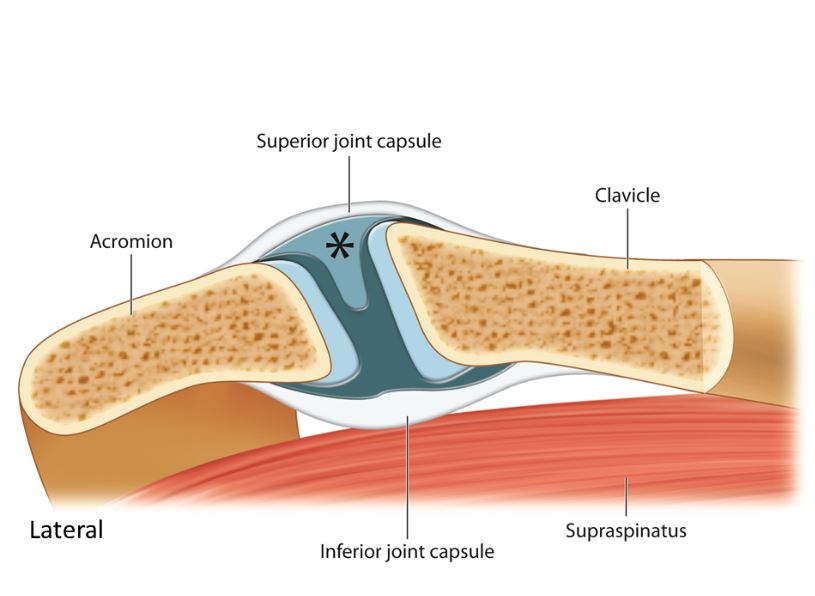 Figure 3. The acromioclavicular joint is a synovial joint with the articular surfaces separated by a wedge-shaped fibrocartilaginous disc (*). The inferior surface of the joint is in direct contact with the subacromial bursa and supraspinatus muscle and may play a role in the development of the impingement syndrome. Reprinted with permission from http://usra.ca.
Figure 3. The acromioclavicular joint is a synovial joint with the articular surfaces separated by a wedge-shaped fibrocartilaginous disc (*). The inferior surface of the joint is in direct contact with the subacromial bursa and supraspinatus muscle and may play a role in the development of the impingement syndrome. Reprinted with permission from http://usra.ca.
The ACJ is a diarthrodial joint located between the concave medial end of the acromion and the convex lateral end of the clavicle, with dual neural innervation from both the suprascapular nerve and the lateral pectoral nerve (Fig. 3). It has limited range of motion, primarily rotation and translation in the anterior-posterior and the superior-inferior planes. The articular surfaces are made up of hyaline cartilage and are separated by a wedge-shaped fibrocartilaginous disk either partly or completely. By early adulthood, the disk is usually little more than a fibrocartilage remnant. The ACJ is stabilized both by static and dynamic stabilizers. Static stabilizers include the acromioclavicular ligaments (superior, inferior, anterior, and posterior), the coracoclavicular ligaments (trapezoid and conoid), and the coracoacromial ligament. Dynamic stabilizers include the deltoid and trapezius muscles.
Sonoanatomy
The patient is positioned sitting or supine with arm neutral because the deep joint space is the widest in this arm positon.[11] A high frequency linear array probe (6-13 MHz) is used for this procedure. The initial scan is obtained with the probe over the joint in the coronal plane (medial part of probe in line with clavicle initially). The probe is then moved anterior-posterior to obtain the best view of the ACJ (hyperechoic ends of acromion, distal clavicle, fibrocartilginous disk, superior joint capsule.
Procedure

 Figure 4. Ultrasound image of the acromioclavicular joint. The upper insert shows the position of the probe and the patient, and the lower insert shows the position of the probe and the structures underneath; A=acromion process; C=clavicle; *=wedge shaped fibrocartilaginous disc; arrow heads=superior joint capsule; SS=supraspinatus muscle. Reprinted with permission from http://usra.ca.
Figure 4. Ultrasound image of the acromioclavicular joint. The upper insert shows the position of the probe and the patient, and the lower insert shows the position of the probe and the structures underneath; A=acromion process; C=clavicle; *=wedge shaped fibrocartilaginous disc; arrow heads=superior joint capsule; SS=supraspinatus muscle. Reprinted with permission from http://usra.ca.
Because the target is superficial, a 25 gauge 1.5 inch needle will be sufficient. The volume of injectate is 1-2 mL of 0.25% bupivacaine with 10-20 mg methylprednisolone acetate), and the approach of needle can be in-plane or out-of-plane (Fig. 4). A few clinical pearls are mentioned here. The ACJ is very shallow and the needle should not be inserted for more than 1 cm deep into the joint. Overzealous injection will deposit medication into the subacromial bursa. One alternative approach for needle insertion is to turn the probe 900 to the standard imaging (from long axis to short axis) and direct the needle in plane from the anterior position. When imaging the ACJ, moving the probe anteriorly may reveal a well-defined cortical discontinuity on the superior aspect of the acromion. This is the “os acromiale,” which is an accessory bone of the acromion that is derived from the non-fused epiphysis of the anterior part of the acromion. The prevalence is approximately 8% and is bilateral in one third of the cases.[12]
Literature review
The accuracy of landmark-based or blind injection for ACJ is limited (40% to 66% in cadaveric studies and 39% to 50% in clinical studies).[5] Accuracy does not differ significantly based on level of experience (specialist, resident, or student).[5] In contrast, accuracy of ultrasound-guided injection ranges between 95% to 100%.[13,14]
The therapeutic role of ACJ steroid injection is unclear as a literature search only reveals a few case series.[15-19] All confirm short term benefit, but response rates are variable. In a certain percentage of patients, the effect can be very long-lasting in terms of years. In a retrospective case series, 27 patients with isolated ACJ arthritis received steroid injections with landmark-based technique.[17] Significant pain relief and functional improvement were achieved in 25 of 27 patients, with a mean duration of improvement of 20 days (range, 2 hrs to 3 months). In another study, 18 patients with isolated unilateral ACJ arthropathy were prospectively studied 2 weeks after ACJ injections were performed under fluoroscopic guidance.18 All patients had pain relief at 2 weeks, with a mean pain score decrease from 7 of 10 to 3.6 of 10 (range, 2-10 and 0-8, respectively). The average duration of pain relief was 14.3 weeks (range, 8-24 weeks). Bain et al15 performed ACJ steroid injection in 44 patients with confirmation of needle placement with fluoroscopy, and the patients were followed up for an average duration of 42 months. Approximately 14% resulted in more than 3 months of pain relief. Hossain et al[16] studied ACJ steroid injections in 25 shoulders from 20 patients prospectively for 5 years. They used the Constant score, which is a composite score of pain and function (total score of 100 points with 15 points in pain assessment), and found that patients continued to improve after 6 months. The average Constant score was significantly better at 5 years than that of preinjection level, with more than 20 point improvement in 72% of the shoulders in the final assessment. The most recent study by van Riet et al19 revealed that only 28% had a clear positive result; but, in most cases, this result was sustained at long-term follow-up (average duration 42 months). There were no complications from the injection.
References
- Pope DP, Croft PR, Pritchard CM, Silman AJ. Prevalence of shoulder pain in the community: the influence of case definition. Ann Rheum Dis. 1997;56:308-312.
- Urwin M, Symmons D, Alison t, et al. Estimating the burden of musculoskeletal disorders in the community: the comparative prevalence of symptoms at different anatomical sites, and the relation to social deprivation. Ann Rheum Dis. 1998;57:649-655.
- Steinfeld R, Valente RM, Stuart MJ. A common sense approach to shoulder problems. Mayo Clin Proc. 1999;74:785-794.
- Burbank KM, Stevenson JH, Czarnecki GR, Dorfman J. Chronic Shoulder Pain: Part II. Treatment. Am Fam Physician. 2008; 77:493-497.
- Peng PWH, Cheng P. Ultrasound-guided interventional procedures in pain Medicine: A review of anatomy, sonoanatomy and procedures. Part III: Shoulder. Reg Anesth Pain Med 2011; 36: 592-605
- Peng PWH. Ultrasound-guided shoulder injection. In: Philip WH Peng (ed). Ultrasound for Pain Medicine Intervention: A Practical Guide. Vol. 4: Musculoskeletal structures. Philip Peng Education Series-iBook series. (Release Feb 2013)
- Hashiuchi T, Sakurai G, Morimoto M, Komei T, Takakura Y, Tanaka Y. Accuracy of the biceps tendon sheath injection: ultrasound-guided or unguided injection? A randomized controlled trial. J Shoulder Elbow Surg 2011; 20:1069-1073
- Zhang J, Ebraheim N, Lause GE. Ultrasound-guided injection for the biceps brachii tendinitis: results and experience. Ultrasound Med Biol 2011; 37:729–733
- Shaffer BS. Painful conditions of the acromioclavicular joint. J Am Acad Orthop Surg. 1999;7:176-188. 15. Henry MH, Liu SH, Loffredo AJ. Arthroscopic management of the acromioclavicular joint disorder: A review. Clin Orthop 1995; 316:276-283.
- Buttaci CJ, Stitik TP, Yonclas PP, Foye PM. Osteoarthritis of the acromioclavicular joint: a review of anatomy, biomechanics, diagnosis, and treatment. Am J Phys Med Rehabil. 2004;83:791-797.
- Park GY, Park JH, Bae JH. Structural changes in the acromioclavicular joint measured by ultrasonography during provocative tests.?Clin Anat. 2009;22:580-585.
- Sammarcoo VJ. Os acromiale: frequency, anatomy, and clinical implications. J Bone Joint Surg Am. 2000;82:394-400.
- Peck E, Lai JK, Pawlina W, Smith J. Accuracy of ultrasound-guided versus palpation-guided acromioclavicular joint injections: a cadaveric study. PM&R. 2010;2:817-821.
- Sabeti-Aschraf M, Lemmerhofer B, Lang S, et al. Ultrasound guidance improves the accuracy of the acromioclavicular joint infiltration:?a prospective randomized study. Knee Surg Sports Traumatol Arthrosc. 2011;19:292-295.
- Bain GI, van Riet RP, Gooi C, Ashwood N. The long-term efficacy of corticosteroid injection into the acromioclavicular joint using a dynamic fluoroscopic method. Int J Shoulder Surg. 2007;1:104-107.
- Hossain S, Jacobs LGH, Hashmi R. The long-term effectiveness of steroid injections in primary acromioclavicular joint arthritis: a five-year prospective study. J Shoulder Elbow Surg. 2008;17:535-538.
- Jacob AK, Sallay PI. Therapeutic efficacy of corticosteroid injections in the acromioclavicular joint. Biomed Sci Instrum. 1997;34:380-385.
- Kurta I, Datir S, Dove M, Rahmatalla A, Wynn-Jones C, Maffulli N. The short-term effects of a single corticosteroid injection on the range of motion of the shoulder in patients with isolated acromioclavicular joint arthropathy. Acta Orthop. Belg. 2005;71: 656-661.
- van Riet RP, Goehre T, Bell SN. The long term effect of an intra-articular injection of corticosteroids in the acromioclavicular joint. J Shoulder Elbow Surg 2012;21: 376-379