CMS Announces “WISeR” Prior Authorization Payment Model for Fee-for-Service Medicare
The Centers for Medicare and Medicaid Services (CMS) has announced a new initiative designed to test prior authorization under the fee-for-service Medicare program. The Wasteful and Inappropriate Service Reduction (WISeR) model will entail hiring contractors to use technology, including artificial intelligence and machine learning, “along with human clinical review,” to manage a prior authorization program for select services.
The initiative marks a significant expansion of prior authorization into Original Medicare, where it has historically been rare. The goal is to reduce “waste, fraud, and abuse,” and CMS hopes to save about $3 billion with the effort. WISeR will be rolled out in specific areas of New Jersey, Ohio, Oklahoma, Texas, Arizona, and Washington over the next six years.
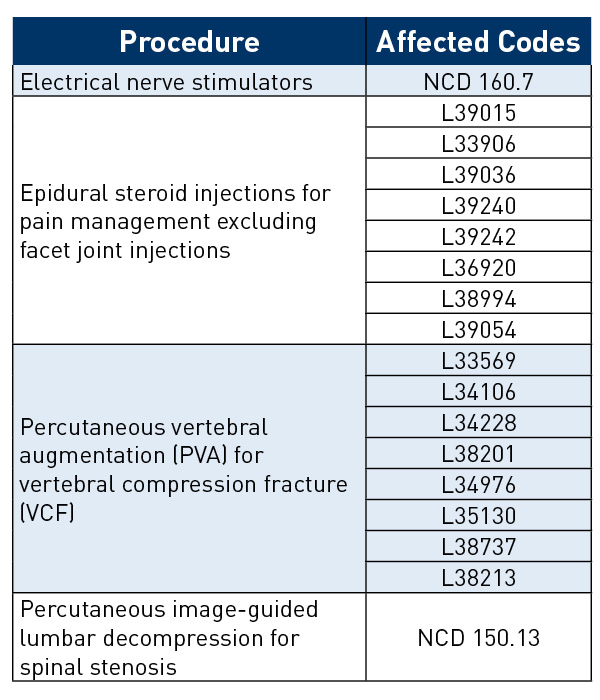
While CMS has indicated a desire to reduce prior authorization burden on doctors and patients, this program could increase administrative oversight for physicians as they adapt to the new processes. Examples of procedures that will be subject to the new model include epidural steroid injections (excluding facet joint injections), electrical nerve stimulators, deep brain stimulation, vagus and sacral nerve stimulation, induced lesions of nerve tracts, percutaneous vertebral augmentation, and percutaneous image-guided lumbar decompression (see table). If successful, the program could be expanded to more services.More than 80% of physicians responding to a recent American Medical Association survey said prior authorization requests—and denials—have increased over the past five years, with an average of 40 prior authorization requests per week.
Providers will be able to choose to submit to the prior authorization requests up front or send claims through pre-payment medical review, the latter of which could cause delays in reimbursement. Contractors will be financially rewarded based on cost savings, which has raised concerns about potential denials for medically appropriate care. Organizations like the American Osteopathic Association also have shared concerns about implementation and additional provider burden.
A fact sheet is available to provide more program details.