Head and Neck Regional Anesthesia Techniques
The head and neck have rich nerve supplies with reliably identifiable surface and bony landmarks. This makes administering regional anesthesia for head and neck surgical procedures practical and effective. Although novel for otolaryngologic surgical procedures, the use of regional anesthesia is commonplace for dental and oralmaxillofacial procedures. Head and neck regional anesthesia is typically employed for postoperative analgesia and placed safely after the induction of anesthesia, but it can also be used effectively as the primary anesthetic (eg, superficial cervical block for carotid endarterectomy). Additionally, patients presenting for head and neck pathology may require awake intubation techniques, and regional nerve blocks can be used to augment local anesthesia topicalization. Finally, regional blocks placed intraoperatively have been used effectively as the sole anesthetic for exploration and hemostasis in the rare and catastrophic event of postoperative bleeding. As with all regional anesthetic techniques, it is important to discuss the planned block with the surgeon preoperatively on a patientby-patient basis as some blocks are contraindicated based on the patient's pathology, covered below. In addition to providing intraoperative and postoperative analgesia, certain blocks can be combined with epinephrine to improve the operative conditions for the surgeon. In the following discussion, we will describe the head and neck blocks typically used in our practice.
Frontal Nerve Block (V1)
The trigeminal nerve, the largest of the cranial nerves, provides sensory and motor innervation to the face. The nerve roots originate in the pons, and the sensory fibers are sent to the trigeminal ganglion. From the trigeminal ganglion, the nerve splits into three major branches: The ophthalmic (V1) nerve, the maxillary (V2) nerve, and the mandibular (V3) nerve.
“Although novel for otolaryngologic surgical procedures, the use of regional anesthesia is commonplace for dental and oral-maxillofacial procedures.”
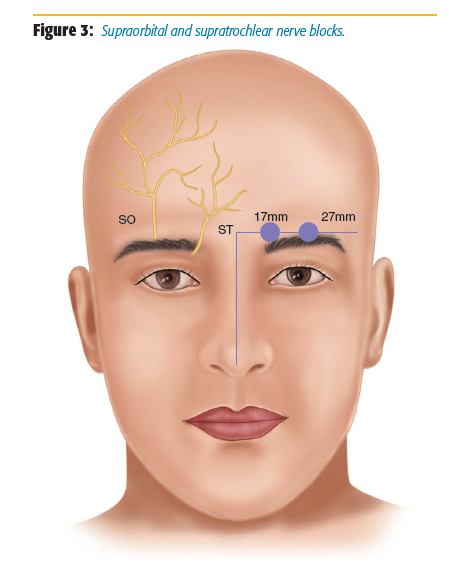
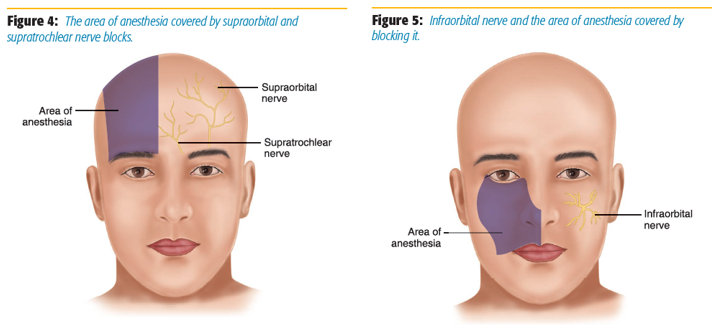
The ophthalmic division of the trigeminal nerve provides pure sensory innervation to the top third of the face (Figure 1). The frontal nerve is the largest branch of the ophthalmic nerve, and it divides into terminal branches called the supraorbital and supratrochlear nerves (Figure 2). The frontal nerve block can be used to block both nerves.[1] These single-shot nerve blocks can be used in ophthalmologic, craniotomies, frontal sinus surgery, and cosmetic nasal surgery. It is performed by palpating the supraorbital notch (located at the middle portion of the superior orbit) and injecting 1–2 ml of 0.5% bupivacaine (blocking the supraorbital nerve) and directing the needle to the medial brow (Figure 3). It is important to palpate the orbit with the free hand and leave a finger on the orbit throughout the block to minimize the risk of injection of local anesthesia into the globe of the eye.[2] The area of anesthesia includes the upper eyelid, forehead, bridge of nose, and scalp (Figure 4).

Infraorbital (V2)
The infraorbital nerve provides sensation to the cheek, upper lip, eyelid, and lateral aspect of the nose (Figure 5). We routinely use bilateral single shot infraorbital blocks combined with bilateral single-shot sphenopalatine blocks for functional endoscopic sinus surgery (FESS) procedures. A randomized study at our institution showed that this block, when combined with a sphenopalatine block, decreases opiate requirements and postanesthesia care unit time.[3] An infraorbital block may also be used for procedures involving the upper lip, nose, and maxillary teeth. Although there are three approaches to block the infraorbital nerve (sublabial, direct, or transnasal), we routinely use a transnasal approach, which reduces the chance of a noticeable facial skin puncture postoperatively.
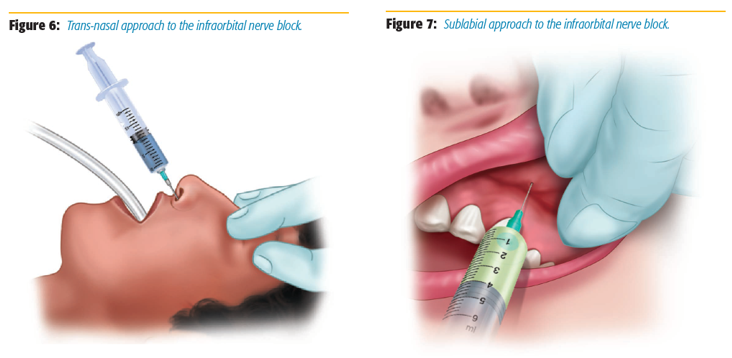
First, the infraorbital foramen, where the infraorbital nerve is located, is palpated by finding the groove located inferior to the orbit rim, 3 cm from the midline of the face.[4] This finger is left in this notch both as a marker for the needle trajectory and also to prevent the needle from entering the orbit. A 1.5-inch 25-gauge needle is inserted through the nares and tunneled superficially under the skin toward the infraorbital foramen, stopping at the halfway point between the edge of the nose and the infraorbital foramen (Figure 6). The needle is then aspirated, and 2 ml of 0.5% bupivacaine is injected.[5] The block is repeated contralaterally for bilateral surgical procedures.
Contraindications to this procedure include neoplasms or arteriovenous malformations involving the nasal cavity. If such contraindications exist, we perform this block using a sublabial approach. In this approach, the free finger is again left on the infraorbital notch for reasons previously mentioned, and the needle is passed starting between the gums and lips until the needle is again positioned midway between the edge of the nose and the infraorbital groove, where the needle is aspirated and 2 ml of 0.5% bupivacaine is injected (Figure 7).[6] If an intraoperative computerized tomography image guidance for FESS is used, this block should be performed after registration because the system uses skin depth, and topography that can be altered by this block.
Infra-Alveolar (Inferior Alveolar Nerve Block, V3)
The mandibular (V3) nerve is the largest branch of the trigeminal nerve. It exits the skull through the oval foramen and then divides into the posterior trunk, which becomes the inferior alveolar nerve that innervates the molar and premolar teeth. This branch travels posterior and lateral to become the lingual nerve along with the inferior alveolar artery and vein, and then exits the mental foramen to become the mental nerve, which provides sensation to the lower lip and chin. The lingual nerve provides sensory innervation to the anterior two-thirds of the tongue, mucosa of the floor of the mouth, and lingual gingiva. Both the inferior alveolar nerve and lingual nerve are blocked concurrently with this block. We use this block for procedures involving the mandible, all mandibular teeth, the floor of the mouth, the anterior two-thirds of the tongue, and the mucosa and skin of the lower lip and chin.
The target for the block is the mandibular nerve as it travels on the medial aspect of the ramus of the mandible, prior to its entry into the mandibular foramen.[7] We use a 25-gauge needle 1.5 inches in length for the single shot. The patient is supine, the mouth is opened, and the cheek is retracted. The coronoid notch and the pterygomandibular raphe are identified.[8] The coronoid notch is the most concave area on the anterior border of the ramus, shown in Figure 8a as the innermost solid blue lines. If not obvious on exam, the notch can be palpated with a finger. The pterygomandibular raphe is indicated by black dashed lines in the same figure.[2] The needle is then placed at the injection site from the contralateral premolar region indicated by the black dot in Figure 8b. The needle is advanced until the mandible is contacted (typically 25–35 mm deep). Once the mandible is contacted, withdraw the needle one millimeter and redirect the needle slightly posterior and inject 2–5 ml of 0.5% bupivacaine. Two to four ml of 0.5% bupivacaine should be injected continuously while the needle is withdrawn to block the lingual nerve.

Sphenopalatine
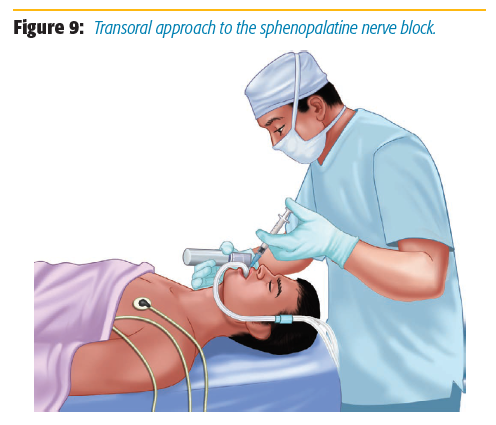
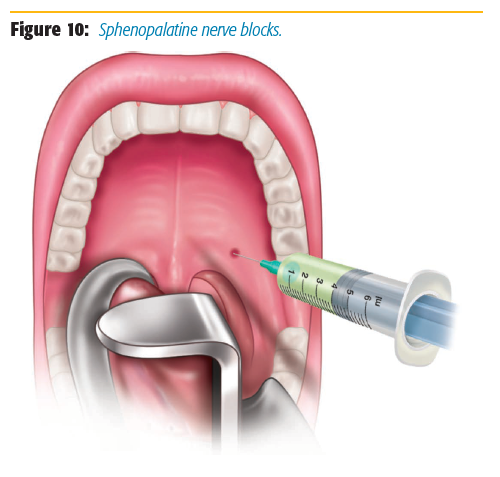
The sphenopalatine ganglion also originates from the maxillary branch of the trigeminal nerve. It provides sensation to the hard palate, soft palate, tonsils, nasal and pharynx mucosa, posterior portion of the nasal septum, and paranasal sinuses. At our institution, we routinely perform a transoral approach to place the sphenopalatine nerve blocks. We perform the block post induction and endotracheal intubation.
After extending the neck, we use a Macintosh 3 blade to sweep the tongue and the endotracheal tube out of the field while illuminating the palate (Figure 9). We identify the greater palatine foramen by locating a groove that is medial to the space between the first and second upper molars (approximately 0.5–1 cm medial). We then use a 1.5-inch 25-gauge needle for injection. The needle is bent at a 90-degree angle at 1.5 cm from the tip and then inserted up to that bend in this groove into the pterygopalatine fossa where the sphenopalatine ganglion is located (Figure 10). The needle is aspirated, and 1.5 ml of 1–2% lidocaine with 1:100,000 epinephrine is injected on each side for bilateral surgical procedures.[5] Localized blanching of the hard palate confirms the correct location when injecting. The blanching is secondary to vasoconstriction of the internal maxillary artery, which is located in the pterygopalatine fossa.[4] Epinephrine added to the local anesthetic helps both decrease absorption in the area as well as improve the surgical field.
Possible complications include intravascular injection, infraorbital nerve injury, and transient diplopia. The sphenopalatine nerve block should be avoided in cases where pathology may involve the pterygopalatine fossa. If the surgeon will be using computed tomography guidance for FESS, this block should be placed before registration because the positioning required for the block (head extension) can disrupt the imaging band on the forehead.
Superficial Cervical Block
The superficial cervical plexus provides sensation from the mandible to the clavicle and can be used for central (thyroid, parathyroid, or thyroglossal cyst) or lateral (neck dissections, lymph node biopsy) surgical procedures. For central procedures, the block is placed bilaterally. If the block will be used for postoperative pain, the landmarks are identified and marked preinduction, and the block is placed postinduction.
While supine, patients are asked to contract their sternocleidomastoid muscle (lift their head against your hand placed on their forehead) to identify the posterior border of the sternocleidomastoid.[2] The flexed muscle seen in the neck contralateral to the direction the patient is pushing is the sternocleidomastoid muscle. The posterior border of this muscle is demarcated with a marker. The midline between the mastoid process and the prominent tubercle of C6 or Chassaignac tubercle at the level of the cricoid cartilage are then demarcated on this border. This midway point is the estimated location of where the cervical plexus emerges.[5-6] The block can be performed either awake or asleep, depending on the procedure and patient preference. Next, a 1.5-inch, 25-gauge needle is used to inject 10 cc of 0.5% bupivacaine superficially along this demarcated border (Figure 11). It is important to remain superficial throughout the injection and to aspirate multiple times during injection to ensure a vessel has not been entered. Risks are minimal for this procedure because the injection is superficial along the border of the muscle. Newer techniques with ultrasound have been described, and several of our faculty use this technique effectively.[9]
Recurrent (Transtracheal) and Superior Laryngeal Blocks
For awake intubations, we routinely perform a transtracheal block to anesthetize the recurrent laryngeal nerves and a direct bilateral superior laryngeal nerve block. We use these blocks to supplement our topicalization of the oropharynx before performing an awake intubation technique, but we also use them for laryngoscopy, bronchoscopy, and transesophageal echocardiography. The superior laryngeal nerve can be blocked at the thyrohyoid membrane (between the superior cornu of the thyroid and the hyoid bone). The superior laryngeal nerve innervates the base of the tongue, the posterior surface of the epiglottis, and the arytenoids.
To perform the block, the patient lies supine and the head is turned away from the side to be blocked. The free hand is used to palpate the hyoid bone or the thyroid cartilage, which can be reliably identified in the majority of patients, and hold it between the index finger and thumb. The superior laryngeal nerve runs slightly lateral to the tubercle of the greater horn of the hyoid bone, and this is the target for the single shot block.[5] The index finger is left on the opposite side of the hyoid, pushing down for hyoid stabilization and identification. A 25-gauge needle is inserted until resistance is felt as it hits the greater horn of the hyoid bone or thyroid cartilage. The needle is then withdrawn 1 mm and checked for negative aspiration, and then 2 ml of 2% lidocaine are injected. This block is done bilaterally.

The recurrent laryngeal or transtracheal block is performed to anesthetize the recurrent laryngeal nerve. The recurrent laryngeal nerve innervates the glottis and the trachea. For the transtracheal block, the patient is positioned supine and the cricothyroid membrane is palpated. A 20-gauge peripheral venous catheter with local anesthesia is inserted into the space while aspirating with a 5-cc catheter until a pop is felt and air bubbles return, confirming position within the trachea. The needle is then removed, leaving the catheter in place to provide immediate access to the airway. A 5-ml syringe filled with 4 ml of 4% lidocaine is reattached and aspirated again to confirm correct position (air bubbles seen on aspiration, negative for blood). The patient is then asked to take a deep breath as the local anesthesia is injected. The patient will typically cough as the local anesthesia coats the vocal cords, so we inform the patient to anticipate this event during consent and again right before we inject.
In addition to being an effective method for anesthetizing the recurrent laryngeal nerve, this technique simultaneously can be used in learning how to perform an emergency needle cricothyrotomy. If this block cannot be performed because of pathology in the area or difficulty in confirming the location, the recurrent laryngeal can also be blocked by inserting an epidural catheter into the fiberoptic scope and injecting 4 ml of 4% lidocaine under direct visualization of the vocal cords.
Conclusion
Despite having described several regional blocks commonly used in our day-to-day practice, this is not an exhaustive list of the nerve blocks for head and neck surgical procedures. By forming strong relationships with the hospital's otolaryngologists over the years, we were able to collaborate and build our current repertoire of regional block techniques. The combination of anatomic and ultrasound-based regional techniques helps us to educate our residents in different techniques for regional blocks. In addition, because our hospital has adopted enhanced recovery after surgery (ERAS) protocols for different surgical procedures, we have incorporated these regional techniques into the head and neck surgery ERAS protocols to attempt to speed recovery and decrease perioperative opioid use.
Acknowledgment
All images are taken with permission from Springer Nature Publishing Rights and Permissions group.
References
- Kanakaraj M, Shanmugasundaram N, Chandramohan M, Kannan R, Perumal SM, Nagendran J. Regional anesthesia in faciomaxillary and oral surgery. J Pharm Bioallied Sci 2012;4:S264–S269. doi: 10.4103/0975-7406.100247
- Levine A.I , DeMaria Jr S. Regional anesthesia. In: Ferraro's Fundamentals of Maxillofacial Surgery. Taub PJ, Patel PK, Buchman SR, Cohen M (eds.). New York, New York: Springer 2015:77–90.
- DeMaria Jr S, Govindaraj S, Chinosorvatana N, Kang S, Levine AI. Bilateral sphenopalatine ganglion blockade improves postoperative analgesia after endoscopic sinus surgery. Am J Rhinol Allergy 2012;26(1):e23–e27. doi: 10.2500/ajra.2012.26.3709
- Levine AI, Govindaraj S, DeMaria S, eds. Anesthesiology and Otolaryngology. Dordrecht, Netherlands: Springer;2013.
- Richardson J. Atlas of interventional pain management. Br J Anaesth 2004;92(4):604–605. doi: 10.1093/bja/aeh544
- Barash PG, Cullen BF, Stoelting RK, Cahalan M, Stock MC. Clinical Anesthesia. 6th ed. Philadelphia, Pennsylvania: Lippincott Williams & Wilkins;2009.
- Khalil H. A basic review on the inferior alveolar nerve block techniques. Anesth Essays Res 2014;8(1):3–8. doi:10.4103/0259-1162.128891
- Takasugi Y, Furuya H, Moriya K, Okamoto Y. Clinical evaluation of inferior alveolar nerve block by injection into the pterygomandibular space anterior to the mandibular foramen. Anesth Prog 2000;47:125–129. https://www.ncbi.nlm.nih. gov/pmc/articles/PMC2149033/ Accessed September 9, 2017.
- Hadzic A, Carrera A, Clark TB, et al. Hadzic's Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia. 2nd ed. New York, New York: McGraw-Hill;2012.

Leave a commentOrder by
Newest on top Oldest on top