Mentorship and Training in RA: How a European Institution Built RA Expertise Through Partnership with a University in the United States
Cite as:
Collaborative Series
A Collaborative Article between ASRA Pain Medicine and European Society of Regional Anaesthesia (ESRA)


Mentoring young anesthesiologists in regional anesthesia is one of those quietly powerful acts that rarely makes headlines but leaves an undeniable mark. Anyone who has ever taken fellows through their first nerve block remembers the look of hesitation, the cautious approach to the probe, the slight tremor in the needle hand, and the surge of satisfaction when the drug tracks perfectly around the nerve. It is an art as much as a science, and like all forms of art, it depends on both technique and trust.
During the past few years, regional anesthesia has exploded with new techniques (eg, erector spinae plane block, quadratus lumborum block, pericapsular nerve group block, suprainguinal fascia iliaca block), and the learning curve has grown steeper. Gone are the days when spinal and transversus abdominis plane blocks were enough to cover the bases. Today’s fellows are expected to navigate complex sonoanatomy, master ever-changing fascial planes, and perform the appropriate blocks in fast-paced enhanced recovery after surgery (ERAS) pathways—often with limited exposure and minimal structured guidance.
We have come to realize that clinical exposure alone does not cut it. Most centers are too busy. Teaching is inconsistent. Residents rotate through services without ever seeing the full continuum of care: pre-block decision making, technical execution, and postoperative follow-up. As such, some institutions have started to do something different: invest in fellows—not just with time or good intentions, but also with money.
Sending fellows to cadaver courses and other workshops and covering their attendance at international congresses are just a few of the ways institutions can financially support the growth of trainees. Yes, it is expensive. A single cadaver course may cost up to €800. Even a short clinical immersion at any high-profile fellowship comes with travel and lodging. But when you look at the impact, it is hard to argue against the value added.
Clinical Immersion
At University Hospitals Leuven, Belgium, we have had the privilege of a long-standing collaboration with the regional anesthesia and acute pain medicine team at Duke University in North Carolina—an exchange born from a shared vision between Admir Hadzic, the Duke team, and Steve Coppins. Each year (except during those difficult COVID-19 years), we have welcomed #DukeRAP fellows to Belgium, and the impact has been profound. These exchanges were funded partly by the fellows, Duke University and the University of Leuven.
For many, it is a truly unique opportunity to experience the fast-paced and innovation-driven setting at Ziekenhuis Oost-Limburg (ZOL) alongside the cutting-edge techniques and educational atmosphere, while also immersing themselves in the academic excellence and multidisciplinary care at Universitair Ziekenhuis Leuven (UZ Leuven). It’s a rare blend of private-sector energy and European academic tradition enriched by expert-led courses, vibrant discussions, and naturally, a taste of Belgian culture (Yes, that includes the beer.).

At ZOL Genk, the practice environment is primarily that of a large peripheral teaching hospital, with a strong tradition in regional anesthesia through its collaboration with New York School of Regional Anesthesia (NYSORA). Much of the focus is on practical application, workshops, and dissemination of techniques to a broad audience of anesthesiologists worldwide. The hospital serves a mixed urban and semi-rural population, with a patient case mix that includes elective orthopedics and general surgery. The style of practice often emphasizes efficiency and reproducibility of regional blocks, making it an attractive training hub for visiting fellows and workshop participants. Academic activity is generally practice-driven with NYSORA acting as a platform for knowledge translation, visual learning, and protocol development.
In contrast, University Hospitals Leuven is Belgium’s largest academic hospital and a leading European reference center. It serves a complex tertiary and quaternary patient population, often with high-acuity cases, advanced oncologic and transplant surgery, and intricate ERAS pathways. Regional anesthesia here is embedded in a fully academic framework with structured fellowships, European Society of Regional Anaesthesia (ESRA) linked initiatives, and formal contributions to international curricula. Practice is research-intensive with numerous RCTs, systematic reviews, and training innovation projects. The hospital’s RA activity is closely connected with education and mentorship at a European level (eg, ESRA, ESRA Academy, cadaver labs, proficiency-based training, etc.)
This collaboration does more than transfer skills—it inspires purpose. It shows young clinicians what’s possible when education is open, international, and visionary. Fellows like James Kim and Amanda Kumar were among the first to take part, and the way their careers have flourished since speaks volumes about the lasting power of mentorship and exchange.
This year, the Belgium team is finally going to do a return visit in October after the American Society of Anesthesiologists annual meeting. We cannot wait!
Workshop, Congresses and Cadaver Courses
At UZ Leuven, we believe that the best way to shape the future of regional anesthesia is to invest directly in the people who will carry it forward. That is why we created a simple but impactful fellows support program, Funding for Fellows (or F3). Every time we give a lecture, host a webinar, or run a scanning session—often with the help of firms or other partners—we set aside an honorarium or other funding. Instead of pocketing it, we put it straight into fellow education. This means that junior colleagues can attend a cadaver course they couldn’t afford, travel to observe another RA team in action, or take part in a congress where they can learn, present, and grow. It is not just about funding but about believing in their potential and creating real chances for them to learn beyond the walls of our own hospital. We are also proud that this model allows for industry support without conflict. There’s no influence on content, no pressure to promote a product—just a shared understanding that education matters. It is a clean and honest way to support young clinicians and keep improving patient care. And frankly, it is one of the most rewarding things we do
/vesalius-cadaver-workshop139b583d-0e9a-4bb6-a781-6749e34726e1.jpg?sfvrsn=7f283b69_1)
There is a tendency in academic medicine to be skeptical of soft returns. What is the evidence? Can we quantify the impact? Are we sure this is not just a nice trip for the fellow? Are we spoiling them and sheltering them from the expenses of the real world when paying for cadaver courses?
In truth, the data are there—if you look beyond randomized controlled trials. A systematic review published in JAMAby Sambunjak et al. (2006) clearly showed that mentorship in academic medicine improves not only career development but also clinical performance and research productivity.1 Another review, in the Journal of General Internal Medicine, emphasized that the quality of mentorship relationships is often what determines whether junior physicians remain engaged in academic or specialized clinical work.2
What about the training itself? A 2020 study by Cale et al. in Medical Science Educator showed that integrating cadaveric review into RA training markedly improved both procedural confidence and anatomic understanding among anesthesia residents.3 Similarly, a study by Niazi et al. (2012) in Regional Anesthesia & Pain Medicine demonstrated that simulation training significantly improved block performance in early-stage learners.4
Granted, cadaver workshops are not yet simulation training. However, modern-day courses have veered away from dissection models to hands-on needle approaches, which are similar to simulation and may be even better. There is also a significant amount of research examining augmented reality, artificial intelligence, needle projection, and other cutting-edge advancements. The future is limitless.
ESRA has played a profoundly transformative role in advancing the practice of regional anesthesia across Europe and beyond. Through the establishment and support of ESRA-approved training centers and by working to benchmark and audit these institutions, ESRA continues to raise the bar in education and clinical excellence.
Equally inspiring is its commitment to equity and opportunity by offering educational grants to promising young professionals with limited resources. ESRA empowers the next generation of regional anesthetists to grow and lead. We owe special recognition to Eleni Moka, whose leadership and vision have helped advance many of these initiatives, amplifying their impact for the greater good.
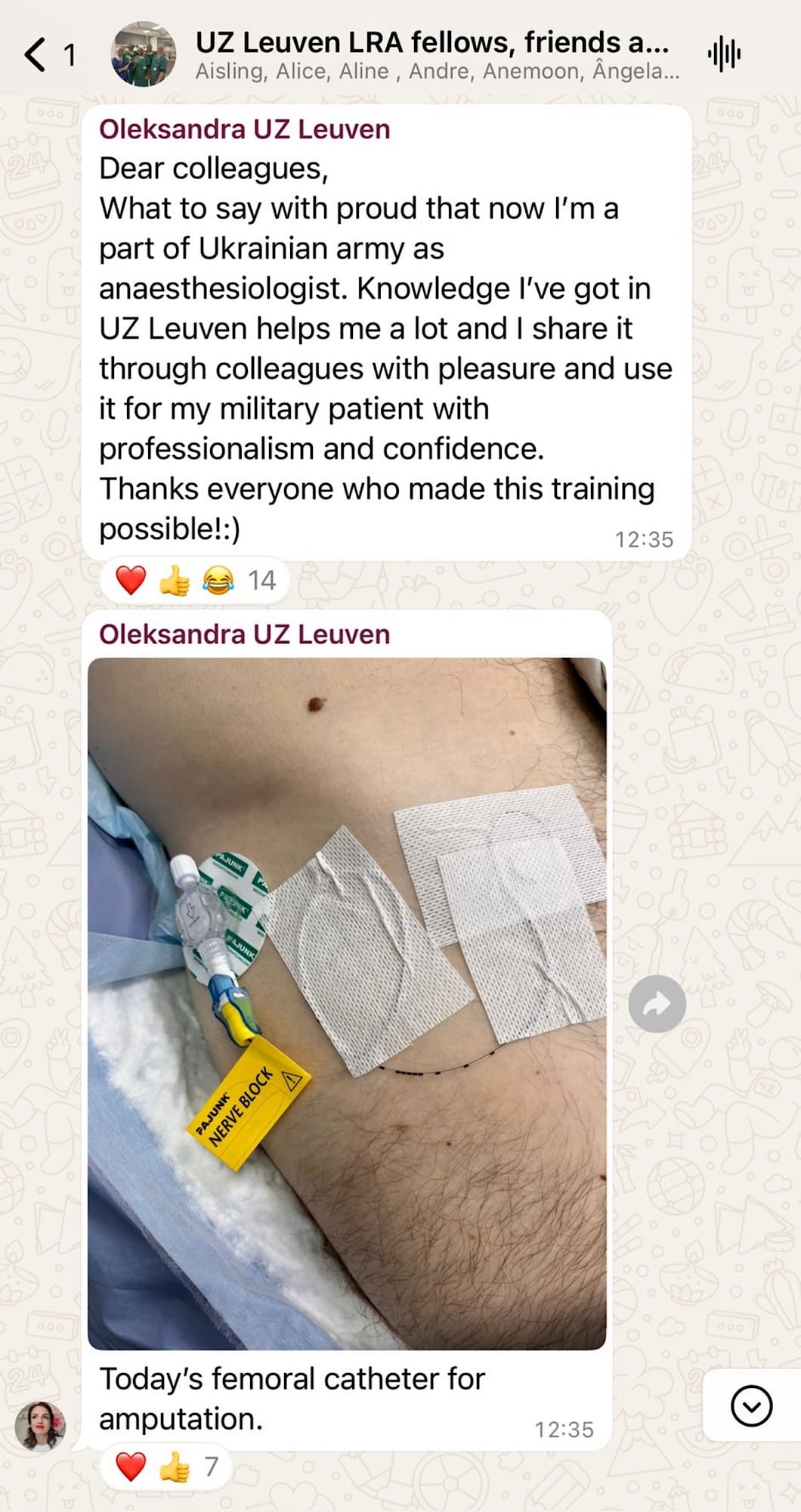
At UZ Leuven, we had the privilege of welcoming Oleksandra, a Ukrainian grant recipient, for a three-month training period. Her journey was especially moving. She met her heroes, Jeff Gadsden and Admir Hadzic, during the Duke exchange in Leuven. Today, she applies the skills acquired from the exchange on the front lines, using regional anesthesia to care for wounded soldiers on the battlefield. Oleksandra is helping improve outcomes in some of the most challenging conditions imaginable.

This is the kind of ripple effect that thoughtful collaboration and meaningful education can achieve, and ESRA continues to be at the heart of it.
More recently, a large European survey by Gisselbaek, Marsh, Soriano, et al. has added depth to this discussion.5 Their study of over 500 anesthesiologists confirmed what many intuitively know: Personal compatibility is the single most important factor in successful mentorship. But it also revealed a troubling undercurrent—women and ethnically underrepresented trainees were significantly more likely to report that potential mentors seemed disinterested. Time constraints were cited, but the perceived lack of access and alignment mattered more. Importantly, both mentors and mentees found these relationships deeply fulfilling when they did work—enhancing not only technical skills but also career confidence and emotional resilience. Although it was a European survey, it was also a nice collaboration with some colleagues from the United States (Samer Narouze, Laura Soriano and Odmara L. Barreto Chang as well as the president of the European Society of Anaesthesiology and Intensive Care, Idit Matot)

So, the message is clear: Structured mentorship, combined with targeted, hands-on learning outside the daily grind of clinical rotations, creates exponential returns. It builds confidence, skill, and professional maturity that can't be rushed between OR turnovers.
What does this look like in practice? In our own center, we’ve adopted a basic but functional model. Every RA-focused fellow receives roughly €1,000 to spend on courses or join a clinical immersion. They are expected to attend one cadaveric course and are encouraged to complete at least one short observership at a center of excellence. Mentors are assigned formally — not just as supervisors, but as career guides. Monthly block debriefs and scan reviews are part of the curriculum. We encourage teaching and strongly support research or poster submissions, even if modest.
What is the result? These fellows stay connected to regional anesthesia long after their rotation ends. They become teachers, auditors, and advocates. Some continue in academic practice; others take these principles back to smaller hospitals and build block services from scratch. All of them practice better medicine. And that, ultimately, is the point.

Investing in people is messier than buying equipment. It doesn’t come with a barcode or warranty. However, it is the only way to create a living, evolving culture of regional anesthesia that will outlast any single machine or technique. When you invest in a fellow—really invest, you are not just teaching blocks. You are shaping the kind of anesthesiologist who can adapt, lead, and pass it on.
And in a field like ours, where the most precise work often happens in the smallest of planes, that kind of legacy is hard to beat.



References
- Sambunjak D, Straus SE, Marušić A. Mentoring in academic medicine: a systematic review. JAMA2006;296(9):1103–15. https://10.1001/jama.296.9.1103
- Sambunjak D, Marušić M, Marušić A. A systematic review of qualitative research on the meaning and characteristics of mentoring in academic medicine. J Gen Intern Med 2010;25(1):72–8. https://10.1007/s11606-009-1165-8
- Cale AS, Hendrickse A, Lyman M, et al. Integrating a cadaver review session into the existing regional anesthesia training. Med Sci Educ 2020;30(2):695-703. https://10.1007/s40670-020-00934-z
- Niazi AU, Haldipur N, Prasad AG, et al. Ultrasound-guided regional anesthesia performance in the early learning period: effect of simulation training. Reg Anesth Pain Med 2012;37(1):51-4. https://doi.org/10.1097/AAP.0b013e31823dc340
- Gisselbaek M, Marsh B, Soriano L, et al. Gender and race/ethnicity dynamics in anesthesiology mentorship: results of a European survey. BMC Anesthesiol 2024;24(1):311. https://doi.org/10.1186/s12871-024-02692-6