A Canadian Perspective of Remote Teaching of Ultrasound-Guided Regional Anesthesia: Providing Equity of Medical Care Around the World
Cite as: Niazi A, Ramlogan R. Collaborative series: A Canadian perspective of remote teaching of ultrasound-guided regional anesthesia: providing equity of medical care around the world. ASRA Pain Medicine News 2025;50. https://doi.org/10.52211/asra080125.003.
Collaborative Series
A Collaborative Article between ASRA Pain Medicine and Canadian Anesthesiologists Society (CAS)
/collab-asra-logo-stacked-in-blue-box-sq.png?sfvrsn=576fe14d_1)

Introduction
The use of ultrasound has revolutionised regional anesthesia. Its use has allowed us to visualize the nerves, the needle approaching the target nerve, and the accurate deposition of local anesthetic. Ultrasonography has improved regional anesthesia block success, quality, and efficiency.1 Ultrasound utilization has also facilitated the education of regional anesthesia.2 However, using ultrasound requires an additional skill set to be taught and practiced. These skills cannot be taught by didactic teaching alone and require practice.3 Guidelines published by the ESRA and ASRA working group have suggested that learning ultrasound-guided regional anesthesia (UGRA) should occur at an accredited continuing medical education event where both didactic and hands-on teaching can occur.3 However, these events are not accessible to all as they are expensive and require traveling and visa requirements. Therefore, many practitioners, especially those in resource-limited countries, cannot access this learning.
Telesimulation
Telesimulation is a remote teaching platform initially defined as “using the internet to connect simulators between an instructor and a trainee in different locations.”4 More recently, McCoy and colleagues5 described it as “a process that combines telecommunication and simulation technologies to deliver education, training, and assessment to learners at a distant location.” Early telesimulation was used by surgeons to teach the fundamentals of laparoscopic surgery,6 by emergency physicians to teach interosseous access,7 and by anesthesiologists to teach UGRA.8 The COVID-19 pandemic spurred more widespread use of this platform to teach many different disciplines.9
Curriculum Development
As ultrasound has introduced new skills that require didactic and hands-on learning, curriculum development for remote teaching of UGRA necessitated the inclusion of both components. Collaborating with our surgical colleagues who had successfully taught the fundamentals of laparoscopic surgery6 we designed a curriculum that divides the teaching into four distinct steps.10 Two steps could be taught didactically, and two required hands-on teaching using a combination of live and simulation models. These steps were 1) image generation, 2) image optimization, 3) image interpretation, and 4) needle insertion and injection.3 The initial didactic step included learning about the basic physics of how the ultrasound machine generates an image; the appropriate selection of transducer; using the gain, focus, depth, and color doppler features; and other functions such as archiving or saving the images and videos. The second didactic step was to optimize the image using different transducer maneuvers. This involved learning about transducer rotation, tilting, applying pressure and properly aligning the probe with the nerve to achieve the best longitudinal or cross-sectional image. The third step required knowledge of anatomy and included identifying the nerve, muscles, blood vessels (differentiating artery from vein), bone and pleura. Learners were also required to know acoustic and anatomical artifacts and ensure no vessels lay in the needle trajectory. The last step included learning the in-plane and out-of-plane techniques of needle insertion and the benefits of each. Competencies included: identifying needle position within the muscle, proper local anesthetic spread, ergonomics and intraneural needle placement.
As ultrasound has introduced new skills that require didactic and hands-on learning, curriculum development for remote teaching of UGRA necessitated the inclusion of both components.
Teaching
The didactic component of the curriculum, which included the first two steps, was taught with a 28-page slide-show presentation that explained the distinctive features of the machine and probes. This included illustrations of the machines with knobology and the differences in using different types of transducers. The third step of scanning was taught by using a live model. The students were encouraged to practice on themselves or their colleagues to develop pattern recognition of the various anatomical structures, and to refine the image acquisition. The last step was taught using a simulation model, similar to our surgical colleagues. It was important that both sites had a similar simulation model so teaching would be translatable; therefore, a simulation model similar to the one we used was shipped or transported to the teaching site. The teaching consisted of two 90-minute sessions and two 90-minute assessments by the learners, which included a pre-test and post-test to determine the impact of the teaching. Sessions were held once a week for four weeks. The students were encouraged to scan themselves and needle the simulation models in between the sessions. The first session consisted of having all the students perform a pre-test, which included the performance of a simulated femoral nerve block, while being assessed. The students were then provided with the slide-show presentation via email and were asked to review this prior to their next session. The third and fourth sessions included scanning and needling and in the final session, the students were asked to perform the simulated femoral nerve block as a post-test. (Figure 1)
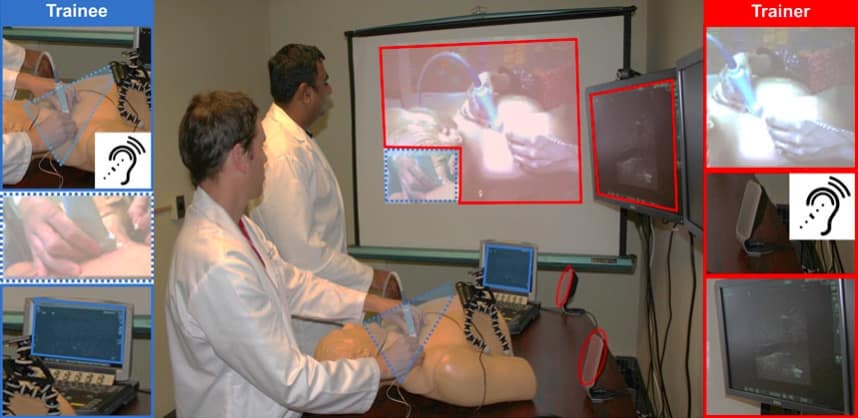
Reproduced with permission from John Wiley and
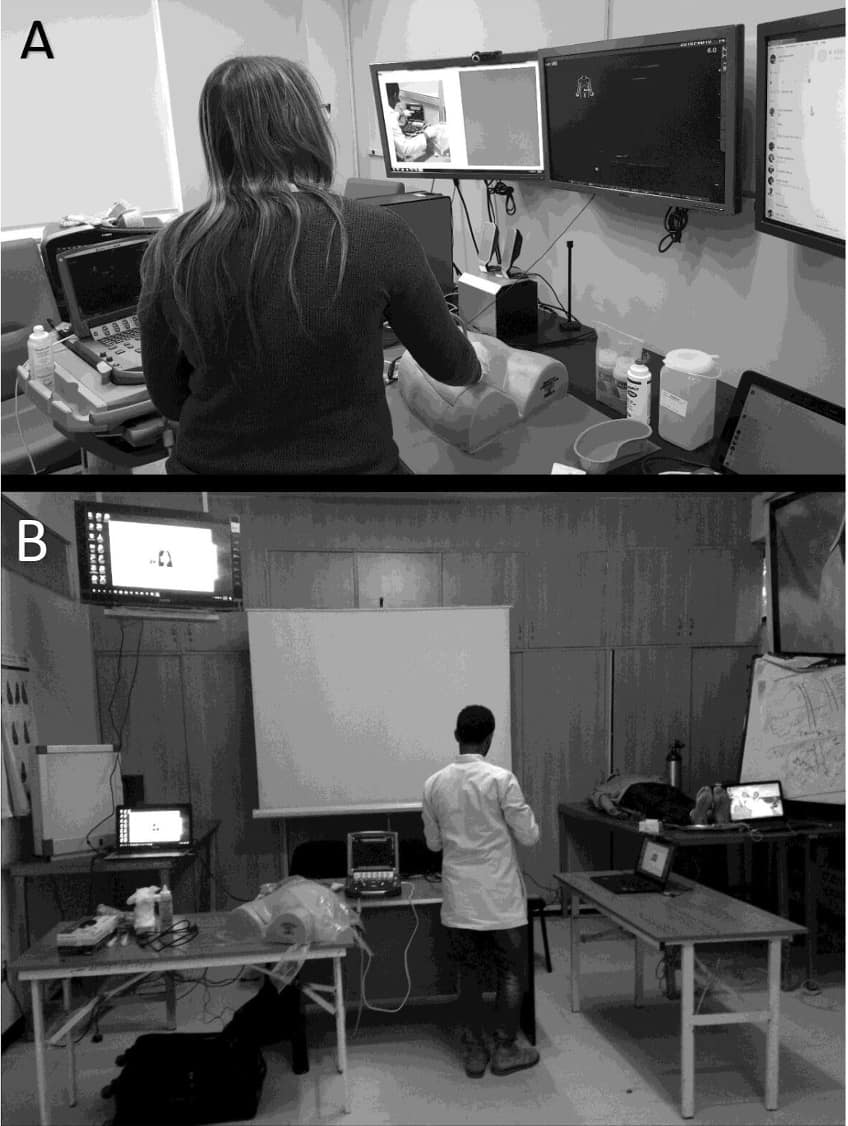
Reproduced with permission from MBJ Publishing Group, Ltd.
Assessment
Remote assessment of the pre-test and post-test was done using a validated scoring system which included a global rating scale (GRS) and a checklist.11 All students were assessed during their pre-test and post-test by raters who were not involved with the teaching. We used both an on-site rater and a remote rater assessing the candidates. A validated modified 20-item procedural Checklist and a 12-item GRS were used, with each participant serving as their own control (Table 1).11 The GRS assessed various aspects of performing a femoral nerve block, including knowledge of equipment, sonoanatomy and local anesthetic, and handling of instruments and tissue. Some points on the GRS were verbally explored to assess the participants knowledge on local anesthetic spread and knowledge of the overall procedure. These aspects were scored 0–5 each, resulting in a maximum score of 60. The Checklist assessed 20 qualities related to scanning, needling and injection techniques, with each quality scored from 0 to 2, giving a maximum score of 40. All students showed significant improvement in their test scores with the post-test total mean score of 84.12 The telesimulation group, consisting of learners located in Ethiopia, rated their learning experience at 7.9 out of a 10-point scale. When asked if they were confident in performing UGRA on a patient, they gave a score of 4.6 out of a 5-point scale. Students gave a 4.3 out of 5 points for recommending the course to a colleague.12
- Proper positioning of the patient
- Correct placement of the ultrasound machine relative to the patient to allow easy visualization of both
- Choice of the correct transducer
- Correct depth, gain, and focal zone choices
- Holds the probe appropriately
- Knowledge or confirmation of screen orientation
- Scanning of anatomy and proper identification of the target
- Use of Doppler to rule out vascular structures (if applicable)
- Appropriate needle alignment
- Maintenance of the needle tip image during advancement of the needle
- Efficiency of regaining the needle tip position image
- Ask for initial aspiration to rule out intravascular injection
- Visualization of the needle tip before injection
- Ask for a 1- to 2-mL initial injection to rule out intraneural and intravascular injection
- Ask the patient or at least look for signs of pain/discomfort
- Ask for proper aspiration every 5-mL increment injection (if applicable)
- Recognition of proper needle tip position
- Perform appropriate needle tip adjustments
- Assessment of ease of injection (high pressure)
- Recognition of correct local anesthetic spread in relation to nerve
*Students received scores of 0 if not performed, 1 if performed poorly and 2 if performed well for each action.11
Preparation for procedure (e.g., monitors, intravenous access, ultrasound machine) | Did not organize the equipment well. Has to stop the procedure frequently to prepare equipment. | Equipment is generally organized. Occasionally, it has to stop and prepare items. | All equipment is neatly organized, prepared, and ready for use. |
1 2 3 4 5 | |||
Patient interaction | Little to no rapport was established; the patient was unaware of the procedures. No sedation is provided. | Rapport is generally established; the patient is aware and informed of most procedures. Patient anxiety is alleviated adequately with sedatives. | Strong rapport is established and maintained throughout the procedure. The patient is well informed of all relevant procedures. Patient anxiety is alleviated through sedation and verbal comforting. |
1 2 3 4 5 | |||
Asepsis (e.g., use of sterile gloves, proper patient draping, probe sterility, cleansing of skin before infiltration, use of op site) | The practice of proper aseptic technique is not generally apparent. Many errors in aseptic technique were made throughout the procedure. | Generally, practice proper aseptic technique. Occasional errors in aseptic technique are made during the procedure. | Excellently demonstrates proper aseptic technique. Few or no errors in aseptic technique were made during the procedure. |
1 2 3 4 5 | |||
Respect for tissue | Frequently uses unnecessary force on the issue or causes damage. | Carefully handles tissue but occasionally causes unintentional damage. | Consistently handles tissues appropriately with minimal damage |
1 2 3 4 5 | |||
Time and motion | Many unnecessary movements. | Efficient time/motion, but some unnecessary movements. | Clear economy of movements. Maximum efficiency. |
1 2 3 4 5 | |||
Instrument handling | Repeatedly makes tentative and awkward movements. | Competent with instruments but occasionally makes awkward or stiff movements. | Fluid movements with instruments and no awkwardness. |
1 2 3 4 5 | |||
Pitfalls and Challenges
Teaching both domestically and internationally presented distinct challenges. Telesimulation relies heavily on technology, including computers, ultrasound machines, video conferencing software, and the internet. Any internet or wireless slowdowns resulted in losing video feed, although audio was maintained, due to the high bandwidth requirements. In resource-limited countries, one major issue was power outages. Despite having reliable internet service, unforeseen power outages would leave us unable to continue our work, as hospital backup generators were mainly required to run the vital areas of the hospital and did not support our equipment outside the operating rooms. These were, however, infrequent. Furthermore, coordinating across different time zones posed a challenge in scheduling mutually convenient times for both tutors and residents outside their clinical commitments. The trainees often struggled to attend sessions due to their clinical duties and were occasionally late, creating time constraints for covering all the material within one session. Overrunning sessions were not feasible, as the venue used by the house staff was frequently booked for other purposes. The 7-hour time difference between sites offered little flexibility for extending sessions. Our teaching sessions started at 0500 hours and finished at around 0630 hours, allowing us enough time to start our working day at 0700 hours. Some sessions could extend beyond the 90 minutes, especially if there were delays in starting and some had to be postponed for another day if there were any technical issues or staffing issues at the teaching hospital.
Telesimulation faces challenges like building rapport, engaging students remotely, and lacking tactile feedback for teaching UGRA. Dynamic camera use was necessary to provide an optimal 3D view of demonstrations. In our studies, follow-up on trainees and the impact on clinical practice were not evaluated. However, it has been shown that sequential didactic lectures and hands-on training improve clinical outcomes.13 Another limitation was that our training was conducted on a simulation model, not a real-time patient. This was technically difficult due to patient consent and the timing of the teaching and its setup. Despite these challenges, evidence suggests simulation-based training enhances technical skills in clinical practice,14-16 and studies in anesthesia further support these findings.17-19
Conclusion
Telesimulation has been demonstrated as a feasible method for teaching UGRA. It can increase the accessibility of UGRA education for physicians in remote areas, enhancing technical skills in clinical practice.


References
- Neal JM, Brull R, Chan VWS, et al. The ASRA evidence-based medicine assessment of ultrasound-guided regional anesthesia and pain medicine. Reg Anesth Pain Med2010;35(Suppl 1):S1-9. https://doi.org/10.1097/AAP.0b013e3181d22fe0
- Sites BD, Gallagher JD, Cravero J, et al. The learning curve associated with a simulated ultrasound-guided interventional task by inexperienced anesthesia residents. Reg Anesth Pain Med2004;29(6):544-8. https://doi.org/10.1016/j.rapm.2004.08.014
- Sites BD, Chan VW, Neal JM, et al. The American Society of Regional Anesthesia and Pain Medicine and the European Society of Regional Anaesthesia and Pain Therapy joint committee recommendations for education and training in ultrasound-guided regional anesthesia. Reg Anesth Pain Med2009;34(1):40-6. https://doi.org/10.1097/AAP.0b013e3181926779
- Roach E, Okrainec A. Telesimulation for remote simulation and assessment. J Surg Oncol2021;124(2):193-9.https://doi.org/10.1002/jso.26505
- McCoy CE, Sayegh J, Alrabah R, et al. Telesimulation: an innovative tool for health professions education. AEM Educ Train2017;1(2):132-6. https://doi.org/10.1002/aet2.10015
- Okrainec A, Henao O, Azzie G. Telesimulation: an effective method for teaching the fundamentals of laparoscopic surgery in resource-restricted countries. Surg Endosc2010;24(2):417-22. https://doi.org/10.1007/s00464-009-0572-6
- Mikrogianakis A, Kam A, Silver S, et al. Telesimulation: an innovative and effective tool for teaching novel intraosseous insertion techniques in developing countries. Acad Emerg Med2011;18(4):420-7. https://doi.org/10.1111/j.1553-2712.2011.01038.x
- Burckett-St.Laurent DA, Cunningham MS, Abbas S, et al. Teaching ultrasound-guided regional anesthesia remotely: a feasibility study. Acta Anaesthesiol Scand2016;60(7):995-1002. https://doi.org/10.1111/aas.12695
- Yasser NBM, Tan AJQ, Harder N,et al. Telesimulation in healthcare education: a scoping review. Nurse Educ Today2023;126. https://doi.org/10.1016/j.nedt.2023.105805
- Niazi AU, Peng PW, Ho M, et al. The future of regional anesthesia education: lessons learned from the surgical specialty. Can J Anaesth2016;63(8):966-72. https://doi.org/10.1007/s12630-016-0653-7
- Burckett-St Laurent DA, Niazi AU, Cunningham MS, et al. A valid and reliable assessment tool for remote simulation-based ultrasound-guided regional anesthesia. Reg Anesth Pain Med2014;39(6):496-501. https://doi.org/10.1097/AAP.0000000000000165
- Liu M, Salmon M, Zaidi R, et al. Ultrasound-guided regional anesthesia: feasibility and effectiveness of teaching via telesimulation in Ethiopia. Reg Anesth Pain Med2021;46(8):722-6. https://doi.org/10.1136/rapm-2020-102394
- Davis D, O’Brien MA, Freemantle N, et al. Impact of formal continuing medical education: do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes? JAMA1999;282(9):867-74.https://doi.org/10.1001/jama.282.9.867
- Stefanidis D, Scerbo MW, Korndorffer JR, et al. Redefining simulator proficiency using automaticity theory. Am J Surg2007;193(4):502-6. https://doi.org/10.1016/j.amjsurg.2006.11.010
- Anastakis DJ, Regehr G, Reznick RK, et al. Assessment of technical skills transfer from the bench training model to the human model. Am J Surg1999;177(2):167-70. https://doi.org/10.1016/s0002-9610(98)00327-4
- Grober ED, Hamstra SJ, Wanzel KR, et al. The educational impact of bench model fidelity on the acquisition of technical skill: the use of clinically relevant outcome measures. Ann Surg2004;240(2):374-381. https://doi.org/10.1097/01.sla.0000133346.07434.30
- Naik VN, Brien SE. Review article: simulation: a means to address and improve patient safety. Can J Anaesth2013;60(2):192-200. https://doi.org/10.1007/s12630-012-9860-z
- Barsuk JH, McGaghie WC, Cohen ER, et al. Use of simulation-based mastery learning to improve the quality of central venous catheter placement in a medical intensive care unit. J Hosp Med2009;4(7):397-403. https://doi.org/10.1002/jhm.468
- Marsland C, Larsen P, Segal R, et al. Proficient manipulation of fibreoptic bronchoscope to carina by novices on first clinical attempt after specialized bench practice. Br J Anaesth2010;104(3):375-81. https://doi.org/10.1093/bja/aeq005